Management of Sepsis: What’s New in 2024?
Sepsis is a clinical syndrome resulting from a dysregulated host response to infection with a severity that ranges from sepsis to septic shock results in life-threatening organ dysfunction. Septic shock represents the most severe form of sepsis, which is characterized by significant drop in systolic blood pressure, with reducing tissue perfusion pressure and leads to the hypoxia typical of shock.
Mortality rates vary but are estimated at >10% for sepsis and > 40% when septic shock is present. This blog covers the management of sepsis and septic shock following guidelines that are largely aligned with established protocols.
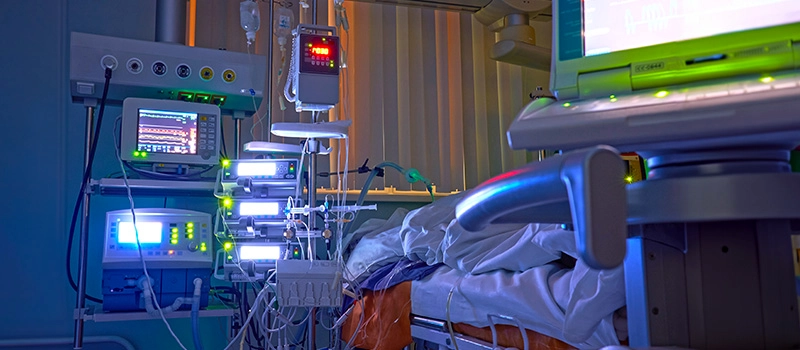
Immediate Evaluation and Management of Sepsis
Managing patients with sepsis and septic shock, it is important to secure the airway, address hypoxemia, and establish venous access promptly to begin administering and antibiotics.
Key steps in the management of sepsis are undertaken simultaneously where possible and comprise:
Resuscitation
The standard airway, breathing and circulation approach to resuscitation is undertaken. Bundles of care are defined by the Surviving Sepsis Campaign.
Airway and Breathing
Immediate intubation and ventilation may be necessary where there is airway obstruction, respiratory failure or impaired consciousness. Extreme care is required when intubating a septic patient because induction of anaesthesia may induce profound hypotension and even cardiac arrest. After intubation, a lung protective ventilation strategy is used.
Circulation
Management of circulation is the immediate priority at presentation. Check heart rate and blood pressure. Perfusion can be impaired in the absence of hypotension and is assessed as follows:
- Clinical signs such as capillary refill time or mental confusion.
- Urine output-measured hourly.
- Lactate- measured by blood gas analysers from an arterial, venous or capillary blood sample. Elevated lactate may reflect anaerobic metabolism due to inadequate oxygen delivery to the tissues (exacerbated if there is reduced lactate clearance by the liver).
- Sample is taken from Central Venous Catheter (CVC) to evaluate in a blood gas analyser.
| Surviving Sepsis Campaign Proposes Two Bundles | |
| To be completed within 3 hours |
|
| To be completed within 6 hours |
|
- Specific devices used to assess the adequacy of intravascular volume replacement and cardiac output.
Fluid Therapy
Fluid is the management of sepsis, helps to restore and maintain adequate tissue perfusion and oxygen delivery to organs.
- Restore Perfusion: Patient experience hypotension and hypoperfusion due to vasodilation and capillary leakage, fluids help to improve blood pressure and increase cardiac output.
- Correct Hypovolemia: Sepsis leads to fluid loss from blood vessels into tissues and fluid therapy replenishes this loss.
- Optimize Organ Function: Adequate fluid resuscitation therapy ensures vital organs like the heart, kidneys, and brain receive enough blood and oxygen.
Types of Fluids
| Crystalloids |
|
| Colloids |
|
| Monitoring and Adjusting Fluid Therapy |
|
| Potential Risks |
|
In recent guidelines mentioned, early and aggressive fluid resuscitation is emphasized, there’ also a shift towards early de-escalation of fluids once stabilization is achieved, especially in Intensive care unit settings.
Vasoactive Drugs
Vasoactive drugs used in sepsis management:
| Norepinephrine (Levophed) |
|
| Vasopressin |
|
| Epinephrine (Adrenaline) |
|
| Dobutamine |
|
Diagnosis of Sepsis
With thorough history and examination, looking for symptoms (e.g. productive cough) and signs like pyrexia or rash, which may suggest the presence of sepsis in patient and the likely primary site of infection.
Target investigations include laboratory tests and radiological imaging to give information on the site of infection.
The initial diagnosis of sepsis CRP may have a role in assessing resolution of infection or failure of therapy by following trends in levels.
Samples for microbiological culture are taken from all potential sites of infection before antibiotic administration when possible, including sputum, urine, CSF and pus depending on clinical presentation.
Antibiotic Administration for Sepsis
Delay between presentation and administration of antibiotics in sepsis will increase mortality.
Antibiotic administration given immediately after cultures have been taken, within one hour of presentation.
General principle is to initiate therapy with broad spectrum agents chosen depending on site of infection, local antibiotic sensitivity patterns, tissue penetration and patient factor such as renal dysfunction.
Results of cultures will enable narrowing of the spectrum of antibiotic therapy, reducing the selection of drug-resistant species such as MRSA and clostridium difficile.
Conclusion
Sepsis remains a major clinical challenge, requiring prompt recognition and effective treatment. In 2024, new advancements focus on early detection through biomarker identification, immunomodulation therapies, and targeted antimicrobial strategies. For MBBS students and healthcare professionals preparing for exams like NEET PG and INI CET, DigiNEET offers expert-led video lectures on the latest updates in sepsis management, including recent treatment protocols and guidelines. DigiOne also provides a strong foundation in Physiology, which is essential for understanding the systemic effects of sepsis and the mechanisms behind organ dysfunction. With interactive quizzes, case studies, and MCQs, DigiNEET ensures students are up-to-date with the latest sepsis management practices and prepared for competitive exams and real-world clinical situations.
Frequently Asked Questions (FAQs)
Q1. What is the sepsis 6 protocols?
Ans. A set of six tasks including oxygen, cultures, antibiotics, fluids, lactate measurement and urine output monitoring- to be instituted within one hour by non-specialist practitioners at the frontline.
Q2. What is the 3-hour protocol for patients with sepsis?
Ans. Four 3-hour SSC guideline recommendations: 1) obtain blood culture before antibiotics, 2) obtain lactate level, 3) administer broad-spectrum antibiotics, and 4) 30 mL/kg of crystalloid fluid administration for hypotension (defined as mean arterial pressure (MAP) < 65) or lactate (> 4).Four 3-hour SSC guideline recommendations: 1) obtain blood culture before antibiotics, 2) obtain lactate level, 3) administer broad-spectrum antibiotics, and 4) 30 mL/kg of crystalloid fluid administration for hypotension (defined as mean arterial pressure (MAP) < 65) or lactate (> 4).
Q3. What is the new treatment for sepsis?
Ans. Drotrecogin alfa (activated) is a new therapeutic agent approved for reduction of mortality in adult patients with severe sepsis or septic shock.
Q5. What fluids are best for sepsis?
Ans. Balanced crystalloids are the fluid of first choice for sepsis resuscitation based on ready availability and taking medication costs into account. Use of 0.9% saline compared to a balanced crystalloid, such as lactated Ringer’s or PlasmaLyte, produces more kidney dysfunction and with a greater risk of dying.
Q6. What is the antimicrobial therapy for sepsis?
Ans. Preferred empiric monotherapy treatment of sepsis includes meropenem, imipenem, piperacillin-tazobactam, or tigecycline. Empiric combination therapy includes metronidazole plus levofloxacin, aztreonam, or a third- or fourth-generation cephalosporin.