DigiNerve is constantly evolving to enhance the user experience while you’re on their journey to becoming a Top Doc. We are excited to bring the latest updates with our commitment to ensure a seamless journey on the go.
Read our monthly newsletter’s September edition (Vol – 2) for the latest updates.
CONTENT UPDATES
PostGrad Course Updates
Dermatology MD:-
1. Chat show on “Scabies and Pediculosis” by Dr. Ragunatha Shivanna, Dr. Priyanka Hemrajani, and Dr. Mariya Babu M. has been added to the course:
Learning Outcomes of the chat show are:
- Understand nature and burden of disease.
- Describe clinical types and clinical features of disease.
- Understand relevance and significance of life cycle of mite and louse in treatment.
- Describe efficacy and safety of therapeutic drugs.
Ophthalmology MD:-
1. Chat show on “Presbyopia Correcting IOLs” by Dr. N. Venkatesh Prajna and Dr. Haripriya Aravind has been added to the course:
Learning Outcomes of the chat show are:
- Indications and contraindications of implanting toric.
- Indications and contraindications of EDOF.
- Indications and contraindications of MFIOLs.
- Factors related to preoperative evaluation, intraoperative pearls and post operative assessment.
Professional Course Updates
Critical Care Simplified:-
1. The panel discussion on “Controversies and Advances in Sepsis” has been added to the module name Sepsis.
Update Your DigiNerve App for Better Experience.
To read the updates shared in the Monthly Newsletter September (Vol-1), click here.
DigiNerve is constantly evolving to enhance your experience while you’re on your journey to becoming a Top Doc. We are excited to bring you the latest updates with our commitment to ensure a seamless journey on the go.
Read on the September edition (Vol – 1) of our monthly newsletter to know the latest updates.
CONTENT UPDATES
PostGrad Course Updates
Dermatology MD:-
1. Benchmark Trials for 108 topics have been updated in the course.
Pediatrics MD:-
1. Chat show on “Approach to a Child with Developmental Delay” by Dr. Piyush Gupta, and Dr. Monica Juneja has been added to the course.
Learning Outcomes of the chat show were:
- Definition and classification of developmental delay
- Screening and diagnosing developmental delay
- Identifying medical and developmental co-morbidities
- Evaluation of risk factors for developmental delay
- Establishing the etiology
Professional Course Updates
MRCOG Part 1:-
1. Webinar on “Acid-base Balance” by Dr. Richa Saxena has been added to the course.
Learning Outcomes of the webinar were:
- Identify, understand, and manage respiratory acidosis
- Understand and manage metabolic acidosis
- Interpret and analyse arterial blood gases (ABGs)
- Recognize, diagnose, and treat respiratory alkalosis
- Diagnose and manage metabolic alkalosis
Update Your DigiNerve App for Better Experience.
Advancements in refractive surgical technology and techniques resulting in the emergence of refractive procedures for patients with myopia, hyperopia, astigmatism, and presbyopia exciting alternatives to traditional spectacles and contact lenses. New methods are being developed to treat eyesight and presbyopia, and modern refractive surgery includes lens-based procedures and laser vision correction (LVC). Improved intraocular lens implant (IOL) technologies that lead to better refractive results and increased independence from spectacles are among the breakthroughs in refractive surgery management. Furthermore, modular IOLs might enable future IOL updates or more flexible vision options. In this blog, we will highlight the broad spectrum of advanced refractive surgical technology for refractive correction where laser treatment has significantly impacted patient care and outcomes.
Types of Surgery for Different Refractive Correction
1. LASIK (Laser in-situ Keratomileusis)
This is a surgery to treat astigmatism, hyperopia, or myopia. Using an excimer laser, the cornea is reshaped during the process. Many earlier refractive eye surgery techniques have been superseded by LASIK. An excimer laser under computer control is used for this procedure. It also makes use of a tiny tool known as a femtosecond laser or microkeratome. The refractive surgeon makes a flap in the cornea’s middle using one of these instruments. The excimer laser is used to remove a thin layer of tissue. The cornea is thus made flat. The flap is swapped out without any sewing. Within minutes, it attaches to the cornea.
An advanced technology for evaluating blurred vision in the eye is wave-front-guided LASIK. The eye can be examined with this technology before surgery. It gauges the amount of distortion that occurs to light as it enters the eye and is reflected. By doing this, an optical map of the eye is produced, highlighting any issues. A LASIK surgeon can perform a more accurate operation by adjusting the laser beam settings thanks to wave-front vision enhancement technologies. This can improve vision and lessen issues with night vision.
2. Photorefractive Keratectomy (PRK)
The aim of photorefractive keratectomy, or PRK, is to treat astigmatism, farsightedness, and nearsightedness by reshaping the cornea using an excimer laser without requiring the creation of a corneal flap. PRK is a surgical procedure that takes five to fifteen minutes to execute for each eye. PRK is usually not painful, though some pressure may be felt throughout the process. The eye is made numb before the surgery using anesthetic drops. The patient is instructed to fixate on a target light while a device holds their eyelid open during the operation. After excising the cornea’s outermost layer, known as the corneal epithelium, the surgeon utilizes an excimer laser to restructure the cornea using computer-controlled light pulses.
3. Radial Keratotomy (RK)
To flatten the cornea, a surgeon performs a refractive keyhole operation (RK). As an excessive curvature of the cornea is generally the cause of myopia, this technique should assist to lessening nearsightedness and astigmatism.
Surgeons frequently operate on one eye using RK before postponing surgery on the other eye for up to six weeks. This pause enables the surgeon to keep an eye on the first eye and document the visual outcome. The surgeon’s technique for operating on the second eye is frequently influenced by the refractive outcome of the first eye’s operation. To provide more equal and consistent vision between the eyes, the patient will be fitted for contact lenses for the uncorrected eye in the interim.
4. Astigmatic Keratotomy (AK)
A surgical procedure known as a limbal relaxing incision, or astigmatic keratotomy (AK), is used to treat astigmatism in the eyes. The cornea’s natural curve is spherical, or basketball-shaped, but astigmatism alters this curvature, giving the cornea an oval or football-shaped shape and misforming its curvature (one end being flat and the other steep). By making one or two incisions at the steepest point of the cornea, AK is a type of corneal relaxing incision surgery that helps correct astigmatism by relaxing the cornea and transforming it into a more rounded shape.
Using a diamond surgical blade, the doctor makes one or two incisions at the steepest point or parallel to the corneal edge while the patient is under topical (anesthetic eye drops) anesthesia.
For improved eyesight, these incisions assist in transforming the cornea’s football-shaped structure into a rounder one.
Typically, the complete process takes no longer than ten minutes for each eye. Even though astigmatism is frequently reduced right after surgery, stability of the effects may not occur for several weeks.
5. Automated Lamellar Keratoplasty (ALK)
An aberrant curvature in the cornea, the transparent front layer of the eye, that keeps light from properly concentrating on the retina, the photosensitive layer at the rear of the eye, and creating a clear image, can be surgically corrected by automated lamellar keratoplasty (ALK). It is recommended for conditions involving aberrant vision, including near- and farsightedness.
Patients are advised to take a break from wearing contact lenses for a while before undergoing ALK. Before the treatment, your cornea’s thickness and visual refractive defects are precisely determined. Local anesthesia is used for ALK procedures. An incomplete flap that is hinged open is created by slicing a layer of the cornea. After that, the underlying cornea is carefully sculpted and incised to correct your eyesight. After that, the flap is sealed and given time to heal naturally. The complete process could take one hour or so. Eye drops are administered to reduce inflammation and soreness while warding against infections. While healing often takes a day or so, clear vision takes several weeks to acquire.
As with any surgery, there is a chance that ALK will result in some consequences. These include infection, glaring of the eyes, scarring, astigmatism (irregular curvature of the cornea), and trouble wearing contact lenses.
6. Laser Thermal Keratoplasty (LTK)
It is a corrective surgical procedure designed to treat farsightedness by reshaping the cornea using a holmium-YAG laser. The objective is to reduce the dependency on corrective lenses, glasses or reading glasses.
This surgery procedure is non-invasive and involves any cutting or tissue removal. Instead, the surgeon utilizes the laser procedure to shrink the collagen fibres which are located on the outer part of the cornea, to steepen it in a controlled manner. This action effectively shifts the focal point of the eye. Because it’s a non-invasive procedure it has minimal risk of complications like infection or vision loss.
However, LTK surgery is not suitable for individuals with refractive instability including those with conditions such as diabetes, lactation, pregnancy, those under age 18 and those using medications such as steroids. Some diseases like rheumatoid arthritis, diabetes, and HIV, which may interfere with wound healing also render individual’s ineligible for LTK. It’s advisable to address these conditions before considering LTK as a treatment option.
7. Small Incision Lenticule Extraction (SMILE)
Ans. SMILE is a single-step, minimally invasive procedure that involves the use of one laser to precisely cut a disc of corneal tissue, which is then removed using a tiny laser incision. Without requiring a cut to the surface of the eye, the entire SMILE treatment is carried out inside the cornea to achieve reshaping. Anesthetic eye drops are used to numb the eye before the surgery. The disc, called a lenticular, is shaped during the process using a laser. The lenticular is then removed using a less than 4mm incision made with the same laser. The femtosecond, or ultra-short pulse, laser used by the SMILE laser doesn’t burn or harm nearby tissue.
The whole SMILE process typically takes 30 seconds, and the incision heals in a few days on its own. SMILE can be used to treat both eyes at once. With SMILE, there is instantaneous final advanced vision correction and a quick recovery with little downtime after the treatment.
Conclusion
E-learning in ophthalmology provides a valuable platform for professionals to stay abreast of the latest advancements in the field of eye care technology. Ophthalmology online courses, offered by esteemed ophthalmologists like Dr. N. Venkatesh Prajna, alongside other online ophthalmology resources, can equip practitioners with the knowledge and skills necessary to deliver exceptional patient care. These platforms provide comprehensive access to up-to-date information on optical innovation diagnostic tools, surgical techniques, and treatment options. By embracing continuous learning through e-learning resources, ophthalmologists can ensure they are providing their patients with the most effective and evidence-based care.
Frequently Asked Questions (FAQs)
Q1. How does refractive cataract surgery last?
Ans. Some persons may experience a recurrence of some blurriness over time. Age-related changes might occasionally cause this, although it can be fixed. Most patients never lose sight of their LASIK results. After ten years, some people might need to have augmentation LASIK surgery.
Q2. What is laser refractive surgery?
Ans. The term “laser refractive eye surgery” describes the application of laser technology to the correction of refractive problems, including astigmatism (uneven focusing), hyperopia (farsightedness), and myopia (nearsightedness).
Q3. What is the recent advanced eye surgery?
Ans. The most advanced laser eye surgery currently offered is Contoura vision LASIK. Sometimes this process is referred to as Topography-guided Custom Ablation Treatment, or T-CAT. The best eye surgeons in the field have refined the LASIK skills they acquired and selected the most effective instruments for the task. What’s left is T-CAT.
Everything is made for a defined purpose anything which is not intended for further use is termed waste. In the scientific and industrial eras combined with the increasing population, the turnover of products has gone very high increasing the quantum of urban solid waste. With the increased need for health care in a changing society the role of hospitals/nursing homes comes to the forefront.
Hospital waste or types of healthcare waste should include any material generated in healthcare establishments including aqueous and other liquid waste.
Hospital waste means any solid, fluid, or liquid waste material including its container and any other intermediate product which is generated during short-term and long-term care consisting of observational, diagnostic, therapeutic, and rehabilitative services for a person suffering or suspected to be suffering from disease or injury and for parturient or during research of production and testing of biological during immunization of human being.
Types of Healthcare waste facilities are responsible for managing healthcare waste generated within their facilities, as well as waste generated through activities in the community. These facilities must undertake proper segregation, collection, in-house transportation, pre-treatment, and waste storage before handing it over to a Common Bio-medical Waste Treatment Facility (CBWTF) operator.
Therefore, proper management of healthcare waste at these facilities necessitates that all categories of staff understand and adhere to the technical requirements for waste handling as per the Biomedical Waste Management Rules, 2016.
Classifications of Waste Generated from Healthcare Sectors
1. Bio-Medical Waste
It refers to any waste produced during diagnosis, treatment, or immunization of humans or animals as well as related research activities, or during the production or testing of biologicals in health camps. This includes all waste from healthcare facilities that could potentially harm human health or the environment if improperly disposed of. Such waste is considered infectious and must be managed according to the Biomedical Waste Management Rules of 2016 to prevent adverse effects on health or the environment.
Around 10% to 15% of the total waste generated by healthcare facilities constitutes biomedical waste. This category includes materials that have come into contact with patients’ blood, secretions, infected body parts, biological fluids, chemicals, medical equipment, pharmaceutical waste, laboratory discharge, sharp objects like needles and glassware, and plastics.
According to the Biomedical Waste Management Rules of 2016, this waste is categorized into four types based on how it is segregated and color-coded. Each category includes specific types of biomedical waste, as given below:
- Yellow Category
- Red Category
- White Category
- Blue Category
These categories are divided as per the types of waste under each category as follows:
| Category | Type of Waste |
| Yellow | Human Anatomical Waste
Human tissues, organs, body parts, and fetus below the viability period (as per the Medical Termination of Pregnancy Act 1971, amended from time to time). |
| Animal Anatomical Waste
Experimental animal carcasses, body parts, organs, and tissues, including the waste generated from animals used in experiments or testing in veterinary hospitals or colleges, or animal houses. |
|
| Solid Waste
Items contaminated with blood, body fluids like dressings, plaster casts, cotton swabs, and bags containing residual or discarded blood and blood components. |
|
| Discarded Medicine
Pharmaceutical waste like antibiotics, and cytotoxic drugs including all items contaminated with cytotoxic drugs along with glass or plastic ampoules, and vials. Etc. |
|
| Chemical Waste
Chemicals used in the production of biological and used or discarded disinfectants. |
|
| Chemical Liquid Waste
Liquid waste is generated due to the use of chemicals in the production of biological and used or discarded disinfectants, Silver X-ray film developing liquid, discarded Formalin, infected secretions, aspired body fluids, liquid from laboratories, and floor washings, cleaning, housekeeping and disinfecting activities, etc. |
|
| Discarded linen, mattresses, beddings contaminated with blood or body fluid, routine mask & gown. | |
| Microbiology, Biotechnology, and other clinical laboratory waste (Pre-treated) | |
| Microbiology, Biotechnology, and other clinical laboratory waste: Blood bags, laboratory cultures, stocks or specimens of microorganisms, live or attenuated vaccines, human and animal cell cultures used in research, industrial laboratories, production of biological, residual toxins, dishes, and devices used for cultures. | |
| Red | Wastes are generated from disposable items such as tubing, bottles, intravenous tubes and sets, catheters, urine bags, syringes without needles, fixed needle syringes with their needles cut, vacutainers, and gloves. |
| White | Waste Sharps Including Metals
Needles, syringes with fixed needles, needles from needle tip cutters or burners, scalpels, blades, or any other contaminated sharp object that may cause punctures and cuts. This includes both used, discarded, and contaminated metal sharps. |
| Blue | Broken or discarded and contaminated glass including medicine vials and ampoules except those contaminated with cytotoxic wastes. |
2. General Waste
General waste includes all waste other than biomedical waste that has not been in contact with hazardous waste or infectious materials, chemicals, or biological secretions, and does not include sharp objects. This type of waste typically includes:
- Newspaper, paper, and cardboard boxes
- Plastic water bottles
- Aluminum cans from soft drinks
- Packaging materials
- Food containers after removing leftover food
- Organic or biodegradable waste, mainly food waste
- Construction and demolition waste
These general wastes are classified as wet wastes and dry wastes and should be collected separately. The quantity of general waste is around 85% to 90% of the total generated from the facility.
3. Other Wastes
Other wastes include electronic devices such as batteries and radioactive materials that are not classified as biomedical waste. They must be disposed of according to specific regulations: the E-waste (Management) Rules of 2016, the Batteries ( Management & Handling) Rules of 2001, and the rules or guidelines established under the Atomic Energy Act of 1962, depending on the type of waste generated.
Guidelines for Management of Healthcare Waste Categories as per Biomedical Waste Management Rules, 2016
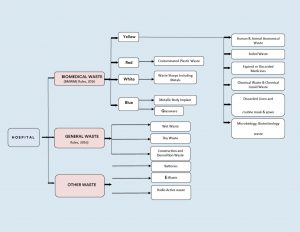
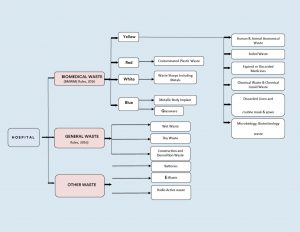
Figure 1: Categorization & Classifications of Wastes in Health Care Facilities.
Color Coding and 4 types of dustbins in hospitals used for Waste Segregation & Collection
According to Schedule I of the Bio-Medical Waste Management Rules of 2016, healthcare facilities (HCFs) must use specific color-coded dustbins and types of containers/bags for segregating and collecting biomedical waste generated within the facility.
| Category | Type of Waste | Colored Container & Type of Container | Treatment Options as per Schedule I |
| Yellow Category |
|
Yellow-colored non-chlorinated Plastic Bags.
NOTE: |
Incineration/deep burial |
| Red Category |
|
Red Colored Non-Chlorinated Plastic Bags (having thickness equal to more than 50u) and containers. | Autoclaving/microwaving/chemical treatment |
| White Category |
|
White Colored translucent puncture-proof, leak-proof, tamper-proof containers. | Autoclaving/microwaving/chemical treatment and destruction/shredding |
| Blue Category |
|
Puncture-proof, leak-proof boxes or containers with blue-colored markings. | Disposal of wastes and secured landfill |
Bio-Medical Waste Collection
Time of Collection
- Daily Collection: Ensure daily collection from each hospital ward at fixed intervals.
- Timing Adjustments: Schedule collections based on waste generation patterns throughout the day.
- Separate Collection: Avoid collecting general waste concurrently with biomedical waste.
- Visitor Waste Management: Collect general waste immediately after visiting hours to prevent accumulation.
- Personal Protective Equipment: Provide PPE to staff handling biomedical waste.
Packaging
- Filling and Sealing: Fill biomedical waste bags and sharp containers up to three-quarters full and seal them promptly.
- Sealing Methods: Use ties or plastic tags to seal bags to avoid stapling.
- Availability of Replacement: Ensure replacement bags or containers are readily available at collection points.
- Labeling Requirements: Label bags and containers with biohazard symbols, including details like date, type of waste, quantity, and sender’s and receiver’s information.
- Barcode Compliance: Affix barcoded labels on the bag as per CPCB guidelines.
Labeling
- Biohazard Symbols: Clearly label all bags, containers, and bins with biohazard or cytotoxic symbols as per BMWM Rules, 2016.




Interim Storage
- Minimization: Discourage interim storage of biomedical waste in patient care areas.
- Designated Areas: Store biomedical waste temporarily in designated, low-traffic areas if necessary.
Treatment Option for Bio-medical Waste Types
| Treatment Options | Biomedical Chemical Processes |
| Thermal Processes Low-heat Systems (93-177oC) |
|
| High-heat Systems |
|
| Mechanical Processes |
|
| Irradiation Processes |
|
| Biological Processes |
|
| Considerations for Processing Incineration |
|
| Autoclaving |
|
| Microwaving |
|
| Deep Burial |
|
| Sharp Materials Disposal |
|
| Radioactive Waste |
|
| Mercury Control |
|
Frequently Asked Questions (FAQs)
Q1. What is clinical waste, and how is it different from infectious waste?
Ans. Clinical waste includes all waste generated from medical facilities, including non-infectious materials like packaging and expired medications, whereas infectious waste refers to waste contaminated with pathogens, such as bacteria, viruses, or other microorganisms.
Q2. What are the proper disposal techniques for biomedical waste, particularly sharps waste?
Ans. Sharp waste like needles and scalpels, must be disposed of in puncture-proof containers specifically designed for sharps disposal. These types of containers are sealed and handled carefully to prevent injuries and potential infections during disposal.
Q3. How does improper medical waste management contribute to the spread of diseases?
Ans. Improper management of biohazardous waste can lead to contamination of the environment and increase the risk of spreading infectious diseases. Pathogens present in medical waste, if not managed correctly, can infect healthcare workers, patients, and the normal public.
Q4. What is some risk associated with inadequate handling of pathological waste?
Ans. Pathological waste which includes tissues, organs, and body parts, poses significant health risks if not properly managed. Exposure to such waste can lead to infections or exposure to hazardous chemicals used in treatments.
Q5. Why is it important for medical facilities to use appropriate medical waste containers?
Ans. Medical waste containers are designed to safely store and transport various types of medical waste, including biohazardous materials and sharps. Using proper containers minimizes the risk of accidental exposure and ensures compliance with regulations for safe disposal.
Cystoid Macular Edema is a condition of the retina in which fluid builds up in the macula central area responsible for clear central vision.
This condition involves ocular inflammation precipitated by cataract surgery, known as pseudophakic CME. It reported incidence after cataract surgery a common complication of 0.1-2.35%.
CME is the most common cause of decreased vision in patients following complicated cataract surgery, occurring much more frequently than either retinal detachment or endophthalmitis. Although CME was clinically recognized and described over 50 years ago much remains unknown about it.
Patients after cataract surgery are at risk for developing CME, a common complicated surgery leading to reduced vision. There are certain demographics that are considered a higher risk, including patients with diabetes, diabetic retinopathy, uveitis, posterior capsule rupture, vitreous prolapse, and previous retinal vein occlusions. Male gender and old age have also been identified as risk factors.
Pathophysiology of Macular Edema
Inflammation plays a large role in the pathogenesis of CME. Pro-inflammatory mediators substances such as Nitric oxide, Vascular Endothelial Growth Factor (anti-VEGF injections), Prostaglandins, cytokines, and other mediators are involved in the inflammatory process that can occur following modern cataract surgery. This inflammation process leads to the destruction of the blood-retinal barrier causing increased vascular permeability. This results in edema of the inner nuclear layer, edema of the outer plexiform layer, accumulation of sub-retinal fluid and ultimately thickening of the retina.
The precise pathophysiology of CME has yet to be fully understood, several factors have been implicated in its development, including vascular instability, vascular traction, and relative ocular hypotony.
CME can lead to permanent vision loss, even after the edema resolves. This is believed to occur due to structural changes in the photoreceptors, which are more prevalent in chronic cases of CME.
Evaluation & Diagnosis
There are different methods for evaluating CME including non-contact and contact slip lamp biomicroscopy, FFA, Fundus stereo photography, indirect ophthalmoscopy, and OCT. Currently, FFA and OCT are the most used investigative tools.
Slit-lamp Biomicroscopy
They are typically conducted using a 78D lens and a 90D lens in the initial step to evaluate macular edema. This microscopic evaluation method reveals the location and presence of macular thickness, exudates, and cystoid changes.
CME is characterized by a unique stellate or radially oriented pattern in the peri-foveal thickness of cysts, attributed to the oblique arrangement of the Henle fiber layer.
Outside the macular region, edema presents a honeycomb appearance caused by the perpendicular alignment of the outer plexiform layer. A central cyst linked to CME may resemble a macular thickness. However, performing the Watzke-Allen test using slit lamp biomicroscopy with a 90D lens reveals an intact vertical without a central break.
Fundus Fluorescein Angiography
FFA can identify areas of retinal capillary leakage. The Early Treatment Diabetic Retinopathy Study (ETDRS) classifies diabetic macular edema into diffuse focal types based on the extent of fluorescein leakage associated with microaneurysms.
According to ETDRS criteria, focal diabetic edema shows 67% or more leakage linked to microaneurysms, intermediate exhibits 33% TO 66% leakage, and diffuse displays less than 33% leakage associated with microaneurysms.
In the early phase of fluorescein angiography, choroidal fluorescence may be partially obscured by significant edema, whether cystoid or non-cystoid especially if the edema is turbid due to lipid-laden macrophages. Dilation of the fine capillary network of telangiectatic retinal vessels around the fovea may be evident in the arteriovenous phase.
In late-phase imaging, hyperfluorescence results from dye leakage from retinal vessels, influenced by the extent of dysfunction in the retinal vascular endothelium. This hyperfluorescence can appear as cystic or irregular staining, filling cystoid spaces rapidly with pronounced leakage or appearing later if leakage is less significant.
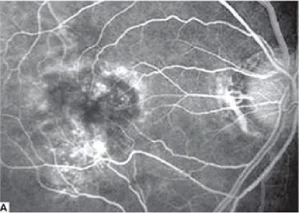
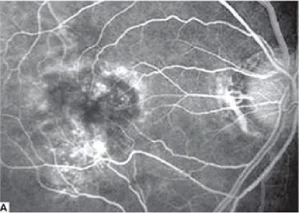
Fig.1.A: Fluorescein angiography shows cystoid macular edema.


Fig.1.B: Clinical photograph shows vitreous incarceration into the wound.
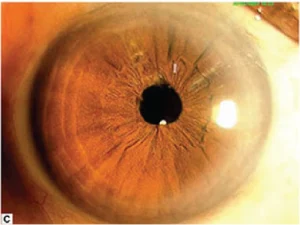
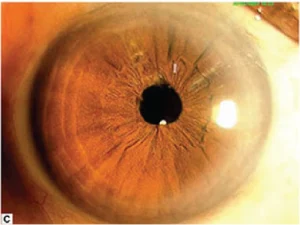
Fig.1.C: Clinical photograph post-vitreolysis.
Cystoid Macular Edema Optical Coherence Tomography (OCT)
Clinicians utilize OCT to assess macular edema stemming from conditions such as age-related macular degeneration, diabetic retinopathy, hereditary retinal degeneration, retinal vein occlusion, edema after cataract surgery, epiretinal membrane, and history of uveitis. Due to its high reproducibility, OCT has emerged as the preferred diagnostic tool for diagnosing and monitoring CME. OCT allows clinicians to identify, locate, and measure fluid accumulations, enabling accurate assessments and ongoing monitoring.
Furthermore, OCT’s ability to categorize different diseases supports prognosis, assists in disease management, predicts patient outcomes, and aids in treatment planning.
- Diabetic Macular Edema: Various patterns of fluid accumulation are visible on OCT scans in patients with diabetic macular edema.
- Diffuse Retinal Thickening: It is defined by retinal thickening exceeding 200um in height and width, featuring regions of reduced reflectivity, particularly noticeable in the outer retinal layers.
- CME: It is characterized by intraretinal fluid accumulation within well-defined spaces of low reflectivity typically around the outer plexiform layer but involving the photoreceptor and inner retinal layers.
- Posterior Hyaloid Traction or Taut Posterior Hyaloid Membrane: This is identified by the presence of a highly reflective membrane on the inner retinal surface, which causes traction and elevation of the retina.
- Subretinal Fluid: It is identified as a dome-shaped dark area situated between the neurosensory retina and the retinal pigment epithelium.
- Tractional Retinal Detachment: This is identified by a peak-shaped retinal detachment caused by traction from proliferative membranes on the retinal surface or within the vitreous. This condition appears as a low signal area beneath the highly reflective border of the detached retina.
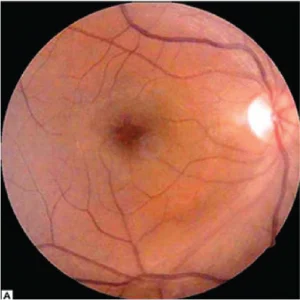
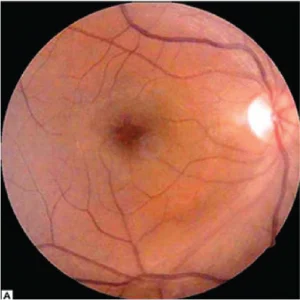
Fig 2.A Color fundus photograph shoes postoperative cystoid macular edema.
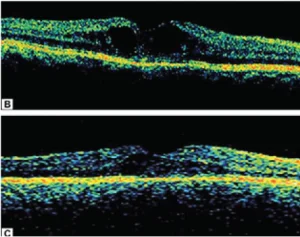
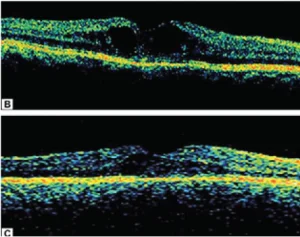
Fig. 2.B Optical coherence tomography shows increased macular thickness with cystoid cavities.
Fig.2. C. Optical coherence tomography shows marked resolution of cystoid space with decrease in macular thickness following sub-Tenon triamcinolone injection.
Radiation Retinopathy
OCT allows clinicians to assess radiation retinopathy using a 5-point grading system, which correlates with visual acuity.
- Grade 1: Foveola-sparing non-cystoid macular edema.
- Grade 2: Foveola-sparing cystoid macular edema.
- Grade 3: Foveola-involving non-cystoid macular edema.
- Grade 4: Mild-to-moderate foveola-involving cystoid macular edema.
- Grade 5: Foveola-involving severe cystoid macular edema.
Juvenile X-linked Retinoschisis
It classifies juvenile X-linked retinoschisis into different types in OCT findings:
- Type 1 or Foveal: Absence of both lamellar schisis on OCT and peripheral schisis on the ophthalmoscopy.
- Type 2 or Foveolamellar: Presence of lamellar schisis on OCT without peripheral schisis on the ophthalmoscopy.
- Type 3 or Complex: Lamellar schisis on OCT and peripheral schisis on the ophthalmoscopy.
- Type 4 or Foveoperipheral: Presence of peripheral schisis on the ophthalmoscopy.
The finding of juvenile X-linked retinoschisis is the presence of a spoke-wheel pattern in the macula, observable in high magnification in patients ages 30 or younger.
On OCT patients with uveitis exhibit diffuse macular edema, CME, and subretinal detachment.
Treatment for Cystoid Macular Edema (CME)
A stepwise medical treatment approach is crucial for managing CME, which involves systemic and ocular pharmaceutical agents. Surgical procedures may also be needed in certain cases.
Systemic Therapy
Many patients develop macular edema as a secondary manifestation of other health conditions such as hypertension, diabetes, dyslipidemia, or inflammatory conditions, it is essential to address these underlying systemic issues.
Some research shows that strict glycemic control can be effective in delaying the onset and progression of diabetic retinopathy in both type 1 and type 2 diabetes.
Intravitreal Anti-Vascular Endothelial Growth Factor
The primary approach for macular edema across various pathologies is intravitreal injections of anti-VEGF agents. Clinicians currently use three formulations of intravitreal anti-VEGF therapies.
Bevacizumab is a 148-kDa humanized full-size monoclonal IgG1 antibody that targets all subtypes of VEGF-A, available in a concentration of 1.25mg/0.05mL.
Ranibizumab offered in concentrations of 0.3mg/0.05mL and 0.5mg/0.05mL, is a 48-kDa humanized monoclonal antibody fragment that targets all subtypes of VEGF-A.
Aflibercept, provided in a concentration of 2mg/0.05mL, is a 115-kDa fusion protein that targets VEGF-A, VEGF-B, and placental growth factors.
Ocular Topical Treatment
Nonsteroidal Anti-inflammatory Drugs
Using topical steroids and NSAIDs prevents prostaglandin synthesis by inhibiting the COX enzyme. Common ocular side effects of topical NSAIDs include burning, stinging, and conjunctival redness. Clinicians should also consider steroid-related adverse effects, such as increased intraocular pressure (IOP), delayed wound healing, and susceptibility to infections.
The latest treatment algorithm for CME, developed by the Jampol lab, involves a combination treatment of typical NSAIDs with topical corticosteroids, such as diclofenac and fluorometholone. If there is no improvement in duration after treatment of 4-6 weeks, an alternative NSAIDS like nepafenac or bromfenac may be prescribed. If vision does not improve after 4-6 weeks of nepafenac or bromfenac treatment, consideration may be given to using an intravitreal corticosteroid injection. Additionally, for cases of treatment-resistant CME, subtenon triamcinolone should be considered as a therapeutic option.
Surgical Treatment for Macular Edema
Vitrectomy is frequently performed for macular edema caused by epiretinal membrane (ERM) thickening of the macula. It is less commonly done for macular edema unless it is related to vitreomacular traction syndromes or taut posterior hyaloid face (TPHC) syndrome, which is often associated with diabetic retinopathy.
Frequently Asked Questions (FAQs)
Q1. What is intraocular lens implantation and how does it improve visual outcome?
Ans. It is a surgical procedure in which a synthetic lens is implanted into the eye to replace the natural lens affected by cataracts. This procedure restores patients’ clear vision by focusing light onto the retina, which results in improving visual outcomes for patients.
Q2. What are some common postoperative complications after uncomplicated cataract surgery?
Ans. Postoperative complications may include temporary discomfort, dry eye symptoms, mild inflammation, and rarely infection. These complications are manageable with postoperative treatment and follow-up care.
Q3. How does diabetes affect cataract surgery and intraocular lens transplantation?
Ans. Cataract surgery outcomes in diabetic patients may influenced by diabetic retinopathy. It requires preoperative assessment, monitoring of retinal thickness, and surgical techniques to achieve optimal results and minimize risks.
Q4. What is the role of subconjunctival injection in postoperative treatment after cataract surgery?
Ans. Subconjunctival injections of medications such as steroids or antibiotics can be used postoperatively to reduce inflammation and prevent infection. It is a localized treatment approach that helps in managing immediate postoperative complications effectively.
Q5. What causes postoperative inflammation after intraocular surgery?
Ans. It includes cataract surgery which is typically triggered by surgical manipulation within the eye. This manipulation can lead to intraocular inflammation characterized by redness, swelling, and discomfort in some patients.
Q6. How common is edema among patients after cataract surgery and what are the risk factors?
Ans. Edema, or swelling of the retina or cornea, can occur after cataract surgery, particularly in patients with diabetes more prone to inflammation. Proper postoperative management including anti-inflammatory treatments, helps mitigate these risks and ensure optimal visual recovery.
The UPSC CMS is an abbreviation for “Union Public Service Commission-Combined Medical Services” Examination. It is a competitive examination that the Union Public Service Commission (UPSC) of India administers. The CMSE is held every year to fill various medical positions in government agencies including the Indian Railways, Central Health Service, Municipal Corporation of Delhi, and several other central government health institutions. The CMS exam allows medical professionals to join the esteemed Indian government healthcare service organizations and support the country’s healthcare system.
The difficulty level of the exam is self-explanatory by the term UPSC; UPSC CMSE is a hard nut to crack. With smart study, consistent efforts, and a lot of practice, you will pass with flying colours. Make sure to start early and stick to a realistic study plan and reliable study resources.
In this blog, you will get detailed information about the UPSC CMS exam recruitment category, eligibility criteria, exam pattern, selection procedure, and syllabus.
To be eligible to sit in the exam, a candidate must be either:
(a) an Indian citizen, or
(b) a subject of Nepal, or
(c) a subject of Bhutan, or
(d) a Tibetan refugee who came over to India before the 1st January 1962 to permanently settle in India, or
(e) a person of Indian origin who has migrated from Pakistan, Burma, Sri Lanka, or East African Countries of Kenya, Uganda, the United Republic of Tanzania, Zambia, 6 Malawi, Zaire, and Ethiopia or Vietnam to permanently settle in India.
Provided that a certificate of eligibility has been issued by the Government of India in favour of the candidate belonging to categories (b), (c), (d), and (e) mentioned above.
UPSC CMS Recruitment Category
UPSC CMS exam is conducted for the recruitment for the following categories and positions:
Category-I:
Medical Officers Grade in General Duty Medical Officers Sub-cadre of Central Health Services
Category-II:
Assistant Divisional Medical Officer in the Railways
General Duty Medical Officer in New Delhi Municipal Council
General Duty Medical Officer Gr-II in Municipal Corporation of Delhi
There are reservations for candidates belonging to Scheduled Castes, Scheduled Tribes, Other Backward Classes, Economically Weaker Sections, and Persons with Benchmark Disability as per the vacancies by the Government.
UPSC CMS Exam Pattern
Medical graduates with an MBBS degree along with completion of internship are eligible to apply for the UPSC CMS exam. There are two parts of CMSE, one is a written examination and the other is an interview. The CMSE comprises two theory papers followed by a personality test or interview. Here’s a breakdown of the exam pattern:
Part-I: Written Examination
The written examination comprises two papers:
Paper-I: This paper includes questions from General Medicine and Pediatrics subject. The exam Pattern 2024 for UPSC CMSE Paper-I is mentioned in the below table:
| Particulars | Details |
| Duration | 2 hours |
| Type of Questions | Objective type Questions (MCQs) |
| Total Marks | 250 |
| Total Number of Questions in Paper I | 120 (96 questions from General Medicine and 24 from Pediatrics) |
| Medium of Question Paper | English |
| Negative Marking | One-third of the marks assigned to a question are deducted for each incorrect answer.
If a candidate gives more than one answer, it will be treated as a wrong answer even if one of the given answers is correct and there will be the same penalty as above for that question. If a question is left blank i.e., no answer is given by the candidate, there will be no penalty for that question. |
Paper-II: This paper includes questions from Surgery, Obstetrics & Gynecology, and Preventive and Social Medicine subjects. The Surgery subject also includes ENT, Ophthalmology, Traumatology, and Orthopaedics subjects. The table below mentions the exam scheme for UPSC CMSE Paper-II 2024:
| Particulars | Details |
| Duration | 2 hours |
| Type of Questions | Objective type Questions (MCQs) |
| Total Marks | 250 |
| Total Number of Questions in Paper II | 120 (40 questions from each subject, Surgery, OBGYN, and Community Medicine) |
| Medium of Question Paper | English |
| Negative Marking | One-third of the marks assigned to a question are deducted for each incorrect answer.
If a candidate gives more than one answer, it will be treated as a wrong answer even if one of the given answers is correct and there will be the same penalty as above for that question. If a question is left blank i.e., no answer is given by the candidate, there will be no penalty for that question. |
Part-II: Interview/Personality Test
After passing the written test, candidates are invited by the Union Public Service Commission for an interview/personality test to determine their fit for the open positions.
The personality test carries 100 marks. The interview is designed to complement the written examination for measuring the general knowledge and academic study skills of the applicants as well as to function as a personality test to evaluate the candidate’s critical thinking skills, absorption capacity, and overall capacity for social cohesiveness, sound judgment, and moral character, initiative, and leadership potential. Basically, it aims to assess the candidate’s personality, communication skills, and suitability for the posts in medical services.
Final Selection
The final selection is done based on the combined marks obtained in Paper-I, Paper-II, and the Interview/Personality test.
Recruitment of a number of candidates is based on the vacancies in the particular position. Succeeding applicants are assigned to different Group-A positions within the public health system. The particular positions and openings change every year.
It’s significant to note that the Paper-I and Paper-II syllabuses contain a broad variety of medical science-related topics. A wide range of medical topics, including clinical disciplines, general knowledge, and current events, are covered in the CMSE curriculum. To score well on the test, candidates must have a solid comprehension of these topics. It is a crucial aspect of a good preparation strategy to know and understand the syllabus of the CMS exam. It leads to effective time management.
UPSC CMS Syllabus
UPSC CMS Syllabus Paper I:
General Medicine subject includes the following topics:
- Cardiology
- Respiratory diseases
- Gastro-intestinal
- Genito-Urinary
- Neurology
- Hematology
- Endocrinology
- Metabolic disorders
- Infections/Communicable Diseases
-
- Virus
- Rickets
- Bacterial
- Spirochetal
- Protozoan
- Metazoan
- Fungus
- Nutrition/Growth
- Diseases of the skin (Dermatology)
- Musculoskeletal System
- Psychiatry
- General
- Emergency Medicine
- Common Poisoning
- Snakebite
- Tropical Medicine
- Critical Care Medicine
- Emphasis on medical procedures
- Patho physiological basis of diseases
- Vaccines-preventable diseases and Non-vaccines preventable diseases
- Vitamin deficiency diseases
- In psychiatry – Depression, psychosis, anxiety, bipolar diseases, and Schizophrenia
Pediatrics subject includes the following topics:
- Common childhood emergencies
- Basic newborn care
- Normal developmental milestones
- Accidents and poisonings in children
- Birth defects and counselling including autism
- Immunization in children
- Recognizing and managing children with special needs
- National programmes related to child health
UPSC CMS Syllabus Paper II:
Surgery subject includes the following topics:
- General Surgery
- Wounds
- Infections
- Tumours
- Lymphatic
- Blood vessels
- Cysts/sinuses
- Head and neck
- Breast
- Alimentary tract
-
- Oesophagus
- Stomach
- Intestines
- Anus
- Developmental
-
- Liver, Bile, Pancreas
- Spleen
- Peritoneum
- Abdominal wall
- Abdominal injuries
- Urological Surgery
- Neurosurgery
- Otorhinolaryngology/E.N.T.
- Thoracic surgery
- Orthopaedic surgery
- Ophthalmology
- Anaesthesiology
- Traumatology
- Diagnosis and management of common surgical ailments
- Pre-operative and post-operative care of surgical patients
- Medico-legal and ethical issues of surgery
- Wound healing
- Fluid and electrolyte management in surgery
- Shock pathophysiology and management
Obstetrics and Gynecology subject includes the following topics:
- Questions on applied anatomy
- Questions on applied physiology of menstruation and fertilization
- Questions on infections in the genital tract
- Questions on neoplasm in the genital tract
- Questions on displacement of the uterus
- Normal delivery and safe delivery practices
- High-risk pregnancy and management
- Abortions
- Intra Uterine growth retardation
- Medicolegal examination in OBGYN including the rape
Family Planning subject includes the following topics:
- Conventional contraceptives
- D. and oral pills
- Operative procedure, sterilization, and organization of programmes in the urban and rural surroundings
- Medical Termination of Pregnancy
Preventive Social & Community Medicine subject include the following topics:
- Social and Community Medicine
- Concept of Health, Disease and Preventive Medicine
- Health Administration and Planning
- General Epidemiology
- Demography and Health Statistics
- Communicable Diseases
- Environmental Health
- Nutrition and Health
- Non-communicable Diseases
- Occupational Health
- Genetics and Health
- International Health
- Medical Sociology and Health Education
- Maternal and Child Health
- National Programmes
- Management of common health problems
- Ability to monitor national health programmes
- Knowledge of maternal and child wellness
- Ability to recognize, investigate, report, plan, and manage community health problems including malnutrition and emergencies.
You can also enroll in online MBBS courses to get conceptual clarity over MBBS subjects by the top medical faculty of India. You have the opportunity to learn and get your concepts clear in Surgery by Dr. Sriram Bhat M, Microbiology by Dr. Apurba S Sastry, Dr. Sandhya Bhat and Dr. Deepashree R, Medicine by Dr. Archith Boloor, Pathology by Prof Harsh Mohan, Prof Ramadas Nayak, and Dr. Debasis Gochhait, and similarly other MBBS subjects by subject’s eminent faculty. The comprehensive knowledge of MBBS subjects and problem-solving capabilities will directly impact your CMS exam.
Frequently Asked Questions (FAQs):
Q1. Is UPSC CMS conducted every year?
Ans. Yes, the UPSC CMS exam is conducted every year and the recruitment is based on the number of vacancies for a particular post in various government health organizations.
Q2. What is a career after CMS?
Ans. UPSC CMSE is conducted for the recruitment of the Medical Officers Grade in General Duty Medical Officers Sub-cadre of Central Health Services, Assistant Divisional Medical Officer in the Railways, General Duty Medical Officer in New Delhi Municipal Council, and General Duty Medical Officer Gr-II in Municipal Corporation of Delhi
Q3. Who conducts the CMS exam?
Ans. The CMS exam is a competitive examination conducted by the Union Public Service Commission (UPSC) of India.
Q4. What is the pattern of UPSC CMS exam?
Ans. There are two parts of CMSE in which part-I is a written examination and the part-II is an interview. The CMSE comprises two theory papers followed by a personality test or interview.
The Part-I written examination comprises two papers: Paper-I and Paper-II.
The National Medical Commission (NMC) has achieved the coveted World Federation for Medical Education (WFME) Recognition Status for a tenure of 10 years. This is a prestigious achievement for India’s medical education. This esteemed award proves NMC’s steadfast dedication to the highest standards in medical education and accreditation.
The WFME recognition will now enable Indian medical graduates to pursue postgraduate training and practice in other countries that require WFME recognition, such as Australia, USA, Canada, and New Zealand.
The World Federation for Medical Education (WFME) is a global organization dedicated to raising the standard of medical education all over the world. The WFME accreditation programme is crucial in ensuring that medical institutions uphold and adhere to the highest levels of global education and training standards.
Dr. Yogender Malik, Member of the Ethics and Medical Registration Board and Head Media Division at NMC, on this remarkable achievement, said, “WFME’s recognition underscores that the quality of medical education in India adheres to global standards. This accolade empowers our students with the opportunity to pursue their careers anywhere in the world, while also making India an attractive destination for international students due to our globally recognized standards.”
Under this accreditation, all the 706 existing medical colleges in India will be considered WFME accredited, and the new colleges being set up in the coming 10 years will also be considered as WFME accredited. This will also benefit NMC in enhancing the quality and standards of Indian medical education by aligning them with global benchmarks. This will facilitate academic collaborations and promote continuous improvement and innovation in medical education.
Now NMC being WFME accredited has opened the doors for all the medical students for ECFMG and USMLE. All Indian students will become eligible to apply for the Education Commission on Foreign Medical Graduates and United States Medical Licensing Examination.
The National Medical Council, Ministry of Health and Family Welfare in a press release dated 20th September 2023 has announced this remarkable update.
Global health comprises the biological and clinical facets of diseases along with the social, economic, political, and environmental determinants of health. The ability to confine health issues inside national borders has diminished as the globe becomes more linked.
The contribution of technology to the medical sector is unparalleled. With the years passing by technology is improving at the highest pace in the medicine sector. Nowadays, the use of AI, and the development of new therapies, drugs, drug development, and surgical procedures, have made complex medical procedures less complex and paved a path to minimally invasive surgeries. Millions of individuals throughout the world are having their lives improved as a result of these developments.
Global health has improved recently despite several obstacles like poverty, pandemics, disease outbreaks, conflicts, and climate change. Maternal and child fatalities have dropped significantly and since the development of new vaccinations, infectious illness spread has also been reduced. Governments and organisations have also boosted their funding for global health concerns and also significantly invested in newer technologies. The current developments in the healthcare industry are beneficial to global health and are an area with significant potential to enhance the health of people all over the world and in the medical field. We can improve the health of people all across the world by addressing the issues and embracing the possibilities.
Medical students and professionals must keep themselves updated and knowledgeable about the recent advancements in healthcare as it is going to impact their career growth to a great extent. To escalate the growth of your medical career, it is mandated to upskill.
The recent advancements in the global healthcare and medicine field are significant for several reasons. By offering more precise diagnoses, earlier illness detection, and more individualised treatment regimens, they have the potential to:
- Improve the quality of care for patients.
- By enabling remote monitoring and care and minimising the need for in-person visits, healthcare may be made more accessible and cheaper.
- Increase the effectiveness of healthcare delivery by simplifying administrative procedures and facilitating information exchange between healthcare professionals.
- Develop novel therapies and preventative measures to lessen the impact of chronic illnesses.
- Boost public health by keeping track of and rapidly and efficiently addressing illness outbreaks.
Below mentioned are technological advancements in medicine and global healthcare:
Artificial Intelligence and Healthcare
With the introduction of unprecedented tools for patient care, treatment, and diagnosis, artificial intelligence (AI) is drastically changing the healthcare industry.
For researchers interested in global health, AI-driven health interventions fall into four categories: diagnosis, patient morbidity or mortality risk assessment, disease outbreak prediction and surveillance, and health policy and planning. Machine learning, signal processing, data mining, natural language processing, and other forms of AI are applied in the healthcare sector.
Here are a few current applications of AI in healthcare:
- Diagnosis and treatment: Artificial intelligence (AI) paves the way for the screening of disease and can analyse medical images like X-rays and scans to identify illnesses early and more accurately than humans. AI may be used to create individualised treatment regimens for individuals based on their unique traits and requirements. Other applications of artificial intelligence being used in medicine include Digital chest radiographs, cervical cancer screening, estimating perinatal risk factors, and characterising and predicting the global spread of the Zika virus.
- Drug discovery: Artificial intelligence (AI) may be used to search through extensive databases of chemicals and compounds to find possible new medicines. AI may also be used to foresee how pharmaceuticals would react in the body, lowering the possibility of adverse effects.
- Personalised medicine: Artificial intelligence (AI) may be used to examine a patient’s genetic information, medical history, and lifestyle choices in order to develop a personalised treatment plan that has the highest chance of success.
- Risk assessment: AI may be used to predict the risk of disease and figure out how likely a patient is to have cancer or heart disease. Patients can utilise this knowledge to guide lifestyle adjustments that will lower their risk.
- Healthcare administration: AI may be used to automate processes like appointment scheduling, patient record management, and claim processing. This might free up medical personnel to concentrate on treating patients.
- Telemedicine: Platforms that employ AI in telemedicine can be used to offer doctor consultations via the Internet. Patients with limited access to healthcare in remote locations may particularly benefit from this.
- Robotics: Surgery, pharmaceutical dispensing, and other medical services can be carried out by AI-powered robots. This might aid in enhancing the effectiveness and precision of healthcare delivery.
- Big data analytics: Using AI, enormous databases of healthcare data may be analysed to spot trends and patterns. The diagnosis and treatment of illnesses can be made better with the use of this knowledge.
- Virtual assistants: AI-driven virtual assistants may be used to set up appointments, answer patients’ inquiries, and offer information about their conditions. The patient experience may be enhanced as a result of this.
The future of AI in healthcare is very promising. The use of AI in healthcare is still in its early stages, but it has the potential to revolutionize the way we diagnose, treat, and manage diseases. In the years to come, as AI technology advances, it is anticipated to have a more significant influence on the healthcare industry.
Advances in Gene Editing Technology
The science of gene editing is expanding quickly. The way we treat illnesses is changing as a result of gene editing tools like CRISPR-Cas9. These technologies can be used to fix genetic flaws that lead to disease or to add new genes that can offer disease protection.
The following are some of the developments in gene editing technologies that are being investigated for medical applications:
- CRISPR-Cas9: A protein called Cas9 is used by CRISPR-Cas9 to cut DNA at a precise spot. This enables precise gene replacement, deletion, and insertion. The most popular gene editing technology, CRISPR-Cas9, is being researched for a number of uses, including the treatment of HIV, cystic fibrosis, sickle cell disease, and hereditary illnesses.
For instance, in cancer patients, CRISPR-Cas9 is being utilised to create novel cancer medicines that can target and eliminate cancer cells. CAR T-cell treatments, a sort of immunotherapy that employs a patient’s immune cells to combat cancer, are being developed by researchers utilising CRISPR-Cas9.
- Base editing: A more recent gene editing technique, base editing allows you to alter specific DNA nucleotides without actually cutting the DNA. Compared to CRISPR-Cas9, this makes it less likely to result in unwanted side effects. For the therapy of conditions including cystic fibrosis and Duchenne muscular dystrophy, base editing is being researched.
- RNA editing: An approach to gene editing that can target RNA molecules rather than DNA. This can be utilised to treat conditions like certain cancers that are brought on by RNA alterations.
- Gene therapy: Gene therapy is a treatment that involves introducing genes into cells to correct a genetic defect. Numerous illnesses, including cancer, HIV, and hereditary ailments, have been treated by gene therapy.
These are only a handful of the gene editing innovations that are being investigated for medical applications. Technology’s continued advancement will probably have a significant influence on how we manage diseases in the years to come.
Development of Precision Medicine
A person’s unique genetic makeup, lifestyle, and environment are all taken into consideration when developing a medical treatment plan in precision/personalised medicine. This may result in a more effective and targeted treatment with fewer adverse effects.
Personalising medicine may be done in a variety of ways. Typical strategies include:
- Genetic testing includes examining a person’s DNA to see if there are any mutations or variances that might impact their likelihood of contracting a certain disease or their reaction to a particular medication.
- Biomarkers are quantifiable indications of a biological condition or state. Biomarkers can be used to monitor a patient’s response to therapy or to spot those who are most likely to catch a particular disease.
- Environmental factors, such as pollutant exposure, food, and exercise impact how people respond to therapy as well as the development of many diseases.
Precision medicine is becoming more and more feasible as we understand more about the human genome and the part genetics plays in disease. We can create more effective and focused therapies that may result in improvement by taking into consideration a person’s particular demands.
Here are some examples of current applications of precision medicine:
- High-risk cancer patients are identified via genetic testing, and targeted medicines are created that are more efficient for those who have certain genetic alterations.
- Biomarkers are being utilised to monitor an individual’s risk of developing heart disease and to pinpoint those who will benefit from certain therapies the most.
- Scientists are examining the genetic component of Alzheimer’s disease and creating targeted treatments that might be more efficient for those who carry particular genetic abnormalities.
Some of the challenges and limitations of precision medicine include cost, accuracy, accessibility, and regulation.
Personalised medicine is a promising subject with the potential to enhance millions of people’s lives despite these difficulties. It is anticipated to become more accessible, inexpensive, and accurate as technology advances.
Development of Telemedicine and Remote Healthcare
Telemedicine and remote healthcare allow patients to receive care from a doctor or other healthcare provider without having to travel to a doctor’s office or hospital. This can help with healthcare access, particularly in remote locations. The COVID-19 pandemic has spurred telemedicine and remote healthcare development to a great extent. These services are increasingly enticing to patients and providers alike because of the requirement to maintain social distance and avoid in-person visits to healthcare institutions. There are several advantages to telemedicine and remote medical care, such as better access to healthcare, lower healthcare expenses, increased patient satisfaction, and better patient results.
Remote healthcare services and telemedicine come in a wide variety. The most popular ones are Tele-education, remote patient monitoring, and virtual doctor appointments.
Additionally, there are several drawbacks to telemedicine and remote treatment, such as security and privacy issues, a lack of financing, technical issues, and a shortage of skilled providers.
Despite these impediments, telemedicine and remote healthcare are expanding quickly and playing a bigger role in the healthcare system. These services are expected to become progressively more common and available as technology advances.
Here are some of the future trends in telemedicine and remote healthcare:
- Increasing the use of artificial intelligence (AI): AI may be applied to personalise treatment regimens, increase the precision of diagnoses, and keep track of patient’s health.
- Development of novel telehealth technology: More thorough and individualised treatment will be feasible thanks to new gadgets like wearable sensors and virtual reality headsets.
- Expansion into new areas: Telemedicine and remote healthcare will be utilised to deliver care in new areas, such as managing chronic diseases and mental health.
Application of 3D Printing in Healthcare
3D printing in medicine is being used to create customised medical items including prostheses, implants, and surgical guides. This innovation might save expenditures while raising the standard of treatment. A rapidly developing technology, 3D printing has a wide range of potential uses in the healthcare sector. Among the most widespread applications of 3D printing in the medical field, some are mentioned below:
- Producing patient-specific medical devices: 3D printing may be used to produce personalised medical items like implants, prostheses, and surgical guides that are tailored to the anatomy of a single patient. In addition to lowering the risk of problems, this can enhance the device’s fit and functionality.
- Building medical models and educating healthcare professionals: 3D printing may be used to build accurate representations of the human body’s organs, tissues, and tumours. These models can be used to aid in the planning and execution of intricate treatments as well as the education of patients about their conditions. This can assist them in picking up new abilities and methods, as well as in practising approaches in a secure setting.
- Creating novel medications and treatments: Tissue scaffolds for cell culture and intricate drug delivery systems may be made using 3D printing. This can aid in the development of novel treatments and medications by researchers for a number of disorders.
- Customising care: Using 3D printing, it is possible to develop treatments and drugs that are specifically suited to the requirements of a certain patient. This might increase the therapy’s efficacy and security.
Here are some specific examples of how 3D printing is being used in healthcare today:
- A company named Materialise has created a 3D-printed breast implant that is specifically designed for women with tuberous breasts. This type of breast deformity is often difficult to treat with traditional implants, but the 3D-printed implant can provide a more natural and comfortable fit.
- A team of researchers at the University of California, San Diego has developed a 3D-printed surgical guide that can be used to remove brain tumors with greater precision and accuracy.
- A company named Organovo has developed a 3D printer that can be used to create human tissue. This tissue can be used to study diseases, develop new drugs, and create personalized medical implants.
These are some of the numerous uses for 3D printing that are now being made in the medical field. As technology advances, it will probably have a bigger influence on the healthcare sector, enhancing the standard of treatment and enhancing accessibility for all.
The use of blockchain technology to increase the security and effectiveness of healthcare data exchange is one of the significant developments being made in the world of healthcare. Smart technologies, particularly wearable sensors, are being developed to extract therapeutically significant health-related data from physical (body) indicators like heart rate, blood pressure, body temperature, respiration rate, and body motion. The technology has now also come up with immersive virtual and augmented reality training and education in the medical field.
Advancements in technology, increased investment in global health, partnerships, collaborations among the government, organizations, and individuals, and innovations altogether make a significant contribution to addressing the challenges to global health and improving health outcomes. The rapid pace of technical improvement has made these developments feasible. These technologies will have a bigger influence on global healthcare as they advance.
The NEET-SS was scheduled for the 9th and 10th of September this year but due to the G20 Summit in New Delhi, the NEET-SS 2023 exam dates have been revised. Now, the revised NEET-SS 2023 exam dates are 29th and 30th September 2023 and it will be conducted at various examination centres across the country.
The NEET-SS 2023 admit card shall now be issued on 22nd September 2023. The NEET-SS 2023 result shall be declared on 15th October 2023.
As per the NBEMS, the revised schedule of NEET-SS 2023 for different groups is as follows:
| Date of Examination | Group | Shift |
| 29th September 2023 | Medical Group | Morning Shift (9 AM to 11:30 AM)
Reporting at Test Centre starts at 7 AM; Entry closes at 08:30 AM |
| 29th September 2023 | Radiodiagnosis Group
Microbiology Group Pathology Group Psychiatry Group Surgical Group Pediatric group Anaesthesiology Group Pharmacology Group |
Afternoon Shift (2 PM to 4:30 PM)
Reporting at Test Centre starts at 12 PM; Entry closes at 01:30 PM |
| 30th September 2023 | ENT Group
Respiratory Medicine Group Obstetrics & Gynecology Group |
Morning Shift (9 AM to 11:30 AM)
Reporting at Test Centre starts at 7 AM; Entry closes at 08:30 AM |
| 30th September 2023 | Orthopaedics Group | Afternoon Shift (2 PM to 4:30 PM)
Reporting at Test Centre starts at 12 PM; Entry closes at 01:30 PM |
The revised schedule for admissions to DM/MCh courses shall be notified in consultation with the National Medical Commission and DGHS (MoHFW).
Know the Reliable Last Minute Tips for the NEET-SS 2023 Exam.
NEET-SS is a National Eligibility cum Entrance Test – Super Specialty, conducted by NBEMS. This year the NEET-SS exam is scheduled on 29th and 30th September 2023. The NEET SS 2023 admit card release date is 22nd September 2023. As the exam is just around the corner, it’s the time for final touchdown with the preparation and getting ready to sit and perform well in the exam.
The blog includes reliable last-minute tips, information regarding admit card and test day procedures, and the documents required to carry for your big day.
Some effective last-minute tips for all the NEET-SS candidates:
Review your notes and flashcards. It is highly advised to stick to your handwritten notes to save much of your time and aid in quick memorization. This will help you solidify your understanding of the topic.
Practice previous years’ papers and practice papers. This will assist you in becoming used to the exam’s format and help you pinpoint any areas that require further practice.
Attempt the Demo exam. To become familiar with the format of the computer-based test, a demo test will be made accessible on the website https://natboard.edu.in. Starting on August 25, 2023, applicants will be able to access the Demo test.
Focus on important and high-yield topics. Prioritize time and focus on the important topics to score high in the exam.
Sleep well the night before the test. You’ll be more awake and concentrated on test day as a result.
On the exam day, have a balanced breakfast. This will keep you energetic and focused throughout the exam.
Be on time for the exam. This will offer you some breathing room and mental preparation time before the exam starts.
Stay calm and focused during the exam. Don’t panic if you don’t know the answer to a question. Just skip it and come back to it later.
Before beginning the exam, carefully read the instructions. This will assist you in avoiding casual errors.
Before you submit your exam, double-check your answers. This will assist you in avoiding any mistakes and you’ll not miss any marks for review questions.
Keep your documents ready and your admit card printed before your exam day to avoid any last-minute chaos.
Here are some more suggestions to control your stress and anxiety:
While studying, take breaks. Avoid being overly worried or overwhelmed by getting up and moving about every 20 to 30 minutes.
Discuss your feelings or problems with a trusted person. This may be a friend, a member of your family, a teacher, or a counselor.
Practice relaxation techniques, such as deep breathing or meditation. You’ll be able to relax and concentrate better as a result.
Keep in mind that anxiety before a test affects everyone. Although feeling anxious is common, try not to let it control you.
Click here to learn about the NEET-SS 2023 exam in detail.
NEET-SS 2023 Admit Card
- The NEET-SS admit card 2023 release date is 22nd September 2023.
- The admit card will be available on the National Board of Examinations in Medical Sciences website and may be notified by SMS/Email alerts and website notice. The candidates will not get an admit card by mail or email.
- It must be downloaded from the NBEMS website and get their admit cards printed. Then, firmly paste the most recent passport-size photograph onto the designated spaces on the card m and adhere to the following requirements:
- Minimum 35×45 mm in size (and no bigger than the space designated on the admit card for pasting the photo), with at least 75% of the photo’s surface area devoted to the head and face.
- The image must be colored with a simple white background.
- A neutral look and a complete frontal view of the face must be shown in the photograph. No caps, stethoscopes, goggles, or additional accessories should be worn.
- The face in the photo shouldn’t have any reflections or shadows on it.
- The photo needs to be printed on high-quality paper with a resolution of at least 600 dpi, and it can’t contain kinks, scratches, or stains.
NEET-SS 2023 Test Day Procedures
- There will be staggered entry as per time slots given in the admit cards and the entry will be done in batches accordingly. Reach the “Reporting Counter” at the exam location at the time specified on the admit card.
- As there are staggered time slots to report, there won’t be a queue at the exam location entrance. Candidates must arrive at the exam site within the time window that will be communicated to them by SMS on their registered telephone number, one day before the exam. The reporting counter will close 30 minutes before the exam starts time. This will give enough time for security checks, identity checks, and examination check-in.
- The admit card mentions the exact street address and location of the test facilities. It is advised to become familiar with the locations of the test centres at least one day before the exam day and make sure to report on time. Please be aware that only candidates who have been granted an admit card will be permitted access to the test centre premises.
- There will be a barcode/QR code reader at the entry gates of the exam centre. It is required to present the admit card and ID proof to the exam functionary who is positioned across with a barcode/QR code reader for verification. The candidates will be made aware of the lab number issued to them.
Things to Carry in the Examination Hall
Printed copy of Barcoded/QR Coded Admit card with the photograph affixed on it.
Photocopy of Permanent SMC/MCI/NMC registration, to be retained by the test centre.
Any one of the following original and valid/non-expired Govt issued photo IDs:
- PAN Card
- Driving License
- Voter ID
- Passport
- Aadhaar Card (with Photograph)
If you want to show an e-Aadhaar card with the Aadhaar number written on it as identity proof, the e-Aadhaar card has to be a high-quality color printout with the photo visible. The picture must be clear and match the candidate presenting the e-Aadhaar Card without any wrinkles, stains, or scratches. In this case, the NBEMS’ decision is definitive.
It is required that the name on the photo identification and the name on the admit card must correspond. It is mandated to present the appropriate paperwork (Marriage Certificate/Divorcee Decree/Legal Name Change paperwork/Gazette notification for name change) to support a claim for change of name if the name has changed as a result of marriage or other circumstances.
I hope these pointers will help you in your NEET SS test preparation. Good fortune!
The Chapter 2 of the NMC Update describes the broad outline of the National Exit Exam, including general features of steps 1 and 2, NExT scores, nature of scores, minimum passing score, etc.
General Features of the NExT Exam
The NExT Exam shall comprise two separate exams referred to as “Steps”.
Step 1: Theoretical Examination
Step 2: Practical/Clinical and Viva Voce Examination
NExT Step 1
1.NExT Step 1 shall be a theoretical and Computer-based/Online examination.
2. It shall comprise one or more types of multiple-choice questions.
3. This shall be a Centralized Common All India Examination that will be held by a body designated by the commission as the conducting authority.
4. The examination shall include six papers covering topics from both Part 1 and 2 of the III MBBS/Final MBBS programme:
- Medicine and allied disciplines
- Surgery and allied disciplines
- Obstetrics and Gynecology
- Pediatrics
- Otorhinolaryngology
- Ophthalmology
(Applied aspects of all subjects covered under I MBBS and II MBBS and Applied aspects of all subjects covered under III MBBS/Final MBBS Part l)
5. Students who have completed their III MBBS/Final MBBS course from a recognized medical college shall be eligible to appear for the examination.
6. NExT Step 1 Examination shall be held twice a year in the months of May and November tentatively.
7. There shall be no restriction on the number of attempts to participate in NExT Step 1 provided that the candidate has completed both the NExT Step 1 and NExT Step 2 exams within ten years of enrolling in the MBBS Course.
8. There is no cap on the number of times for attempting the NExT Step 1 Regular Examination to improve your score but you can only go for the improvement after completing your NExT Step 2.
9. The III MBBS/Final MBBS Part 1 and III MBBS/Final MBBS Part II Practical/clinical examinations will continue to be held conventionally unless otherwise stated by the Commission and the NExT Step 1 will replace the traditional university/institutional Theory Examinations of the III MBBS/Final MBBS Part II.
NExT Step 2
1. The NExT Step 2 shall be a Practical/Clinical and viva voce examination comprising seven clinical subjects/disciplines:
- Medicine and allied disciplines
- Surgery and allied disciplines
- Obstetrics and Gynecology
- Pediatrics
- Otorhinolaryngology
- Ophthalmology
- Orthopaedics and PMR (Physical Medicine and Rehabilitation)
2. The exam shall be objectively structured, clinical case-based, and use simulated cases and patients to evaluate practical and clinical skills as well as clinical decision-making and communication abilities expected of an Indian medical graduate.
3. The exam must be taken in person or live, and it must be administered by the relevant state health universities or institutions in accordance with the norms and directives given by the Commission. The Commission will choose the university or institution that is permitted to conduct NExT Step 2 for the relevant colleges where there are no state health universities.
4. The Regular NExT Step 2 Exam shall be held twice a year.
5. A NExT Step 2 Supplementary Examination is only open to candidates who have failed in one or more (up to three) of the seven subjects and are required to repeat specific subjects. It will be held twice a year. If a candidate fails in more than three subjects, then they will have to appear in supplementary exams of all the seven subjects.
7. As long as the candidate has completed both the NExT Step 1 and NExT Step 2 Examinations within ten years of enrolling in the MBBS programme, there is no restriction on the number of attempts to participate in NExT Step 2.
NExT Scores
1. Nature of Scoring
- The marks in NExT Step 1 must be calculated as a whole number, which will serve as the Raw Scores with the proper decimals. Also, equivalent Percentages (marks out of a maximum of 100) with the proper decimals may then be calculated.
- The outcomes of the NExT 2 exams will only be reported as Pass/Fail depending on the acquisition of the relevant competence that is being evaluated.
2. Minimum scores for passing
- The minimum score to pass shall be 50% of the total or half of the maximum possible Raw for NExT Step 1.
- To pass the NExT Step 1 exam, you must receive a minimum of 50% (50 out of 100) in each of the six papers or half of the maximum possible Raw Scores.
- The requirements for passing NExT Step 2 include a successful demonstration of having acquired the competencies that are evaluated, with a pass/fail result being given.
3. Calculation of NExT Step 1 scores for determining merit for the purpose of admission to Postgraduate courses in broad specialties
- The sum of the raw scores earned in each paper or topic in a single NExT 1 exam will be used to calculate the Total Marks for determining the merit, particularly for admission to broad specialization Postgraduate Courses.
- The candidate must follow the generation of a rank application process as stipulated by the Commission from time to time in order to determine rank for admission into Postgraduate courses in broad specializations in a given academic year. Only individuals who have submitted an application for rank generation will be eligible for admission for that cycle of the academic year.
- The NExT Step results will be valid for five years in order to determine merit, notably for admission to broad-specialty postgraduate courses. If a candidate has appeared in the NExT exam cycle then the score of the latest given NExT step 1 exam will be considered.
- Tie-breaker rule for rank generation:
-
- Normalized sum of raw scores obtained in each paper in NExT step 1 although the method of normalization will be notified later.
- Candidate with the lower attempts in NExT step 1 will be placed higher in the merit list.
- Candidates will be given higher rank based on the higher marks in the following order of preference:
-
-
- Medicine and allied disciplines
- Surgery and allied disciplines
- Obstetrics and Gynecology
- Pediatrics
- Otorhinolaryngology
- Ophthalmology
-
4. Utility of NExT Scores
- An MBBS student from a college recognized by the Commission shall be eligible for compulsory internship only if they pass in each of the six theory papers of NExT Part 1 and also pass in III MBBS/Final MBBS (Part 2) Practical/Clinical Examination.
- A medical student who has completed their undergraduate studies abroad at an institution recognized by the Commission and who has met the necessary requirements outlined in the Commission’s Foreign Medical Graduate Regulations is eligible to participate in the mandatory rotating internship programme only if they pass in all six NExT Step 1 Theory Papers.
- A medical graduate who received their training in India or outside of India will be entitled to register in the Indian Medical Register and State Medical Register and obtain a license to practice modern medicine in India, only if, they have completed the internship for the appropriate length of time and have successfully passed the NExT Step 2 (Practical / Clinical) Examination. You must fulfill all the requirements as per the Registration of Medical Practitioners and Licence to practice Medicine Regulations, of NMC. Also, all the other requirements are considered appropriate by the Commission, Concerned University/Institution and duly applicable at that time.
- For admission to PG medical courses in broad specialty subjects, a candidate must meet the following criteria:
- Candidates must meet the conditions outlined for NExT Part 1 and 2, making them eligible for a license to practice modern medicine in India.
- Must engage in common counselling by a designated authority granted by the Central Government or Commission.
- The NExT Step I Scores may be used by the Government of India, the State Governments, any organization of the Government of India, the State Governments, or any autonomous or private body/institution for the purpose of employment, provided that the necessary authorization has been sought and authorized by the National Medical Commission or other appropriate authorities as determined to be appropriate.
Click Here to Read NMC NExT Exam Update – Chapter 1 (Preliminary)
Click Here to Read NMC NExT Exam Update – Chapter 3 (General Information)
The NExT Exam latest news includes Chapter 1 (Preliminary) and Chapter 2 (Broad Outline) and Chapter 3 (General Information).
The core objective of the NExT exam is to provide consistency in summative evaluations conducted across the nation in relation to the minimal requirements for a medical graduate’s education and training.
The National Exit Test (NExT), shall serve as a licentiate examination for validating a medical graduate’s eligibility to register for practice the contemporary system of medicine in India.
NExT will also act as an entrance exam for admission to PG medical education in broad medical specialties by determining the eligibility and ranking of the MBBS students.
The National Exit Exam shall be applicable to:
- All undergraduate medical students seeking the MBBS degree at all medical colleges that have been accredited by the National Medical Commission along with Institutes of National Importance (INIs) are subject to the National Exit Test (NExT).
- All foreign medical graduates who have been granted approval by the NMC for the purposes of obtaining a license to practice medicine as a registered medical practitioner in India and for enrollment in the State Register or the National Register in such a manner as may be specified by regulations.
- Anyone with a medical degree aiming to pursue an academic course, an observership, or any other purpose that may be specified and allowed by the NMC by appropriate notification or rules from time to time.
- Anyone with the granted medical license practicing in India wishes to pursue PG degree can take the NExT exam.
According to the draft released, the NExT comprises two separate examinations, referred to as “Steps”.
Step 1: Theoretical Examination
Step 2: Practical/Clinical and Viva Voce Examination
The Commission shall from time to time determine, by appropriate regulations and/or notification, the applicable method of employing the NExT results for admission to Postgraduate Courses in wide medical specialties by means of common counselling by the designated authority.
There is no confirmation yet on the academic session to which the NExT exam will be applicable but when it will come into force, all other corresponding and equivalent examinations shall be phased/ceased out.
It is still to be decided by the Commission Central Government, State Government, that the existing examinations, however, shall continue for as long as may be necessary or the analogous existing exams will be replaced by the NExT. The Commission will decide when it is necessary and will notify the use of scores and normalization of various examinations and the NExT, when applicable concurrently, for such purposes as may be appropriate.
Chapters 2 and 3 of the update include the complete structure of the NExT Examination, objectives, exam pattern, eligibility, distribution of subjects, nature of scoring, timetables, and more.
Click Here to Read NMC NExT Exam Update – Chapter 2 (Broad Outline)
Click Here to Read NMC NExT Exam Update – Chapter 3 (General Information)
INI-CET is a combined national-level entrance examination for admission to the medical postgraduate courses – MD, MS, DM (6 yrs), MCh (6 yrs), and MDS at INI institutes (Institute of National Importance). The INI-CET January session 2023 exam is around the corner. Getting admission to INI institutes is highly challenging and a dream for MBBS students. This is a highly competitive task to secure a seat in the renowned medical colleges in India.
Remember, Perseverance is the key.
The INI-CET exam is going to be held on 13th Nov 2022 for admission to the AIIMS INI-CET January session 2023.
Mode and Scheme of INI-CET January 2023 exam
| Particulars | Description |
| Mode of Examination | Computer-based test (CBT) |
| Duration | 3 hours (180 minutes) |
| Number of questions | 200 |
| Types of questions | Objective type |
| Marking Scheme | +1 mark for every correct response and -1/3 for every incorrect response |
Important things to know:
- If more than one candidate scores the same, then this tie-breaker situation is resolved by applying the following criteria sequentially:
-
- Less negative marks
- Older by age
- Candidates equal to 8 (eight) times the number of postgraduate seats available in each category will be called for the first and second rounds of seat distribution based on the INI-CET merit list.
- Spot Round Counseling will only be conducted if the seats will remain vacant even after the open round counseling.
List of Participating Institutes for INI-CET January 2023 Session
| S. No. | Name |
| 1 | AIIMS, New Delhi |
| 2 | AIIMS, Bhopal |
| 3 | AIIMS, Bhubaneswar |
| 4 | AIIMS, Jodhpur |
| 5 | AIIMS, Nagpur |
| 6 | AIIMS, Patna |
| 7 | AIIMS, Raipur |
| 8 | AIIMS, Rishikesh |
| 9 | AIIMS, Bibinagar |
| 10 | AIIMS, Bhatinda |
| 11 | AIIMS, Deoghar |
| 12 | AIIMS, Mangalagiri |
| 13 | AIIMS, Raebareli |
| 14 | JIPMER, Puducherry |
| 15 | NIMHANS, Bengaluru |
| 16 | PGIMER, Chandigarh |
| 17 | SCTIMST, Trivandrum |
Here’s the tentative seat distribution (Category-wise) for admission to various MS/MD/DM (6 years)/MCh (6 years)/MDS courses at AIIMS, New Delhi and other 12 AIIMS through the INI-CET entrance examination for the January session of 2023.
Table 1: Tentative seat distribution for INI-CET January 2023 session at AIIMS, New Delhi:
| Courses | Subject/Specialty | Total Number of Seats | UR | OBC | SC | ST | EWS |
| MD | Anaesthesiology | 17 | 7 | 5 | 3 | 1 | 1 |
| MD | Anatomy | 5 | 2 | 1 | 1 | 1 | 0 |
| MD | Biochemistry | 8 | 4 | 2 | 1 | 1 | 0 |
| MD | Biophysics | 8 | 3 | 2 | 1 | 1 | 1 |
| MD | Community Medicine | 9 | 5 | 2 | 1 | 0 | 1 |
| MD | Dermatology & Venerology | 5 | 1 | 2 | 1 | 0 | 1 |
| MD | Emergency Medicine | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Forensic Medicine | 4 | 1 | 1 | 1 | 0 | 1 |
| MD | Geriatric Medicine | 3 | 1 | 1 | 1 | 0 | 0 |
| MD | Lab. Medicine | 5 | 2 | 1 | 1 | 0 | 1 |
| MD | Medicine | 11 | 5 | 3 | 2 | 0 | 1 |
| MD | Microbiology | 5 | 2 | 1 | 1 | 0 | 1 |
| MD | Nuclear Medicine | 4 | 3 | 0 | 0 | 0 | 1 |
| MD | Obstetrics & Gynecology | 11 | 4 | 3 | 2 | 1 | 1 |
| MD | Ophthalmology | 6 | 3 | 1 | 1 | 1 | 0 |
| MS | Orthopaedics | 4 | 1 | 1 | 1 | 0 | 1 |
| MS | Otorhinolaryngology | 5 | 1 | 1 | 1 | 1 | 1 |
| MD | Pediatrics | 10 | 3 | 3 | 2 | 1 | 1 |
| MD | Palliative Medicine | 4 | 3 | 1 | 0 | 0 | 0 |
| MD | Pathology | 10 | 4 | 3 | 1 | 1 | 1 |
| MD | Pharmacology | 6 | 1 | 2 | 1 | 1 | 1 |
| MD | Physical Medicine & Rehabilitation | 2 | 2 | 0 | 0 | 0 | 0 |
| MD | Physiology | 10 | 5 | 2 | 1 | 1 | 1 |
| MD | Psychiatry | 4 | 1 | 1 | 1 | 0 | 1 |
| MD | Radiodiagnosis & Internventional Radiology | 4 | 1 | 1 | 1 | 1 | 0 |
| MD | Radiation Oncology | 4 | 3 | 1 | 0 | 0 | 0 |
| MS | Surgery | 8 | 3 | 2 | 1 | 1 | 1 |
| MD | Transfusion Medicine | 5 | 2 | 2 | 1 | 0 | 0 |
| MDS | Conservative Dentistry & Endodontics | 1 | 0 | 1 | 0 | 0 | 0 |
| MDS | Pediatrics & Preventive Dentistry | 2 | 0 | 1 | 0 | 0 | 1 |
| MDS | Prosthodontics | 1 | 0 | 1 | 0 | 0 | 0 |
| MCh | Neuro Surgery M.Ch (Direct 6 year Course) | 2 | 2 | 0 | 0 | 0 | 0 |
| MCh | Paediatric Surgery M.Ch (Direct 6 year Course) | 2 | 2 | 0 | 0 | 0 | 0 |
| DM | Infectious Diseases DM(Direct 6 year Course) | 4 | 4 | 0 | 0 | 0 | 0 |
Table 2: Tentative seat distribution for INI-CET January 2023 session at AIIMS, Bhopal:
| Courses | Subject/Specialty | Total Number of Seats | UR | OBC | SC | ST | EWS |
| MD | Anaesthesiology | 6 | 5 | 1 | 0 | 0 | 0 |
| MD | Anatomy | 1 | 0 | 0 | 1 | 0 | 0 |
| MD | Biochemistry | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Community Medicine | 5 | 2 | 1 | 0 | 1 | 1 |
| MS | ENT | 3 | 1 | 1 | 1 | 0 | 0 |
| MD | Forensic Medicine & Toxicology | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | General Medicine | 3 | 1 | 0 | 1 | 0 | 1 |
| MS | General Surgery | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Microbiology | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Obstetrics & Gynecology | 3 | 1 | 0 | 1 | 1 | 0 |
| MD | Ophthalmology | 3 | 1 | 1 | 0 | 0 | 1 |
| MS | Orthopaedics | 4 | 2 | 1 | 1 | 0 | 0 |
| MD | Pediatrics | 4 | 2 | 1 | 0 | 1 | 0 |
| MD | Pathology | 4 | 1 | 1 | 1 | 0 | 1 |
| MD | Pharmacology | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Physiology | 1 | 0 | 0 | 1 | 0 | 0 |
| MD | Psychiatry | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Radiodiagnosis | 4 | 1 | 2 | 0 | 0 | 1 |
| MD | Radiotherapy | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Transfusion Medicine & Blood Bank | 2 | 0 | 0 | 1 | 1 | 0 |
Table 3: Tentative seat distribution for INI-CET January 2023 session at AIIMS, Bhubaneswar:
| Course | Subject/Specialty | Total Number of Seats | UR | OBC | SC | ST | EWS |
| MD | Anaesthesiology | 9 | 3 | 2 | 2 | 1 | 1 |
| MD | Anatomy | 7 | 3 | 2 | 2 | 0 | 0 |
| MD | Biochemistry | 3 | 1 | 0 | 1 | 1 | 0 |
| MD | Community Medicine | 5 | 2 | 1 | 1 | 0 | 1 |
| MD | Dermatology | 3 | 1 | 1 | 0 | 1 | 0 |
| MD | Emergency Medicine | 5 | 2 | 1 | 1 | 1 | 0 |
| MS | ENT | 3 | 1 | 1 | 1 | 0 | 0 |
| MD | Forensic Medicine & Toxicology | 5 | 2 | 1 | 1 | 1 | 0 |
| MD | General Medicine | 3 | 2 | 0 | 0 | 0 | 1 |
| MS | General Surgery | 6 | 2 | 2 | 1 | 0 | 1 |
| MD | Microbiology | 2 | 1 | 0 | 1 | 0 | 0 |
| MD | Nuclear Medicine | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Obst. & Gynecology | 6 | 3 | 1 | 1 | 0 | 1 |
| MD | Ophthalmology | 2 | 0 | 1 | 1 | 0 | 0 |
| MS | Orthopaedics | 6 | 4 | 1 | 0 | 0 | 1 |
| MD | Pediatrics | 5 | 2 | 1 | 1 | 1 | 0 |
| MD | Pathology | 5 | 2 | 1 | 1 | 0 | 1 |
| MD | Pharmacology | 4 | 1 | 1 | 1 | 0 | 1 |
| MD | Physiology | 6 | 2 | 1 | 1 | 1 | 1 |
| MD | PMR | 2 | 1 | 0 | 0 | 0 | 1 |
| MD | Psychiatry | 4 | 1 | 0 | 1 | 1 | 1 |
| MD | Radiodiagnosis | 3 | 2 | 0 | 0 | 1 | 0 |
| MD | Radiotherapy | 3 | 1 | 1 | 0 | 0 | 1 |
| MD | Transfusion Medicine | 3 | 1 | 1 | 1 | 0 | 0 |
Table 4: Tentative seat distribution for INI-CET January 2023 session at AIIMS, Jodhpur:
| Course | Subject/Specialty | Total Number of Seats | UR | OBC | SC | ST | EWS |
| MD | Anaesthesiology & Critical Care | 17 | 6 | 5 | 3 | 1 | 2 |
| MD | Anatomy | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Biochemistry | 3 | 1 | 1 | 0 | 0 | 1 |
| MD | Community Medicine | 6 | 2 | 2 | 1 | 1 | 0 |
| MD | Dermatology & Venerology | 3 | 1 | 1 | 1 | 0 | 0 |
| MD | Emergency Medicine | 4 | 2 | 1 | 1 | 0 | 0 |
| MD | Forensic Medicine & Toxicology | 4 | 2 | 1 | 0 | 1 | 0 |
| MD | General Medicine | 4 | 2 | 1 | 1 | 0 | 0 |
| MS | General Surgery | 7 | 2 | 2 | 1 | 1 | 1 |
| MD | Microbiology | 6 | 2 | 2 | 1 | 0 | 1 |
| MD | Nuclear Medicine | 3 | 1 | 1 | 0 | 1 | 0 |
| MD | Obstetrics & Gynaecology | 5 | 2 | 1 | 1 | 0 | 1 |
| MD | Ophthalmology | 4 | 2 | 1 | 1 | 0 | 0 |
| MS | Orthopaedics | 5 | 2 | 1 | 0 | 1 | 1 |
| MS | Otorhinolaryngology | 6 | 2 | 1 | 1 | 1 | 1 |
| MD | Paediatrics | 8 | 3 | 2 | 1 | 1 | 1 |
| MD | Pathology | 7 | 2 | 2 | 1 | 1 | 1 |
| MD | Pharmacology | 3 | 2 | 1 | 0 | 0 | 0 |
| MD | Physiology | 4 | 2 | 1 | 1 | 0 | 0 |
| MD | PMR | 4 | 2 | 1 | 1 | 0 | 0 |
| MD | Psychiatry | 5 | 2 | 1 | 1 | 0 | 1 |
| MD | Radiology | 5 | 2 | 1 | 1 | 0 | 1 |
| MD | Transfusion Medicine & Blood Bank | 2 | 1 | 1 | 0 | 0 | 0 |
| MCh | Paediatric Surgery (M.CH. 6 Years) | 2 | 2 | 0 | 0 | 0 | 0 |
| DM | Radiation Oncology (D.M. 6 Years) | 2 | 2 | 0 | 0 | 0 | 0 |
Table 5: Tentative seat distribution for INI-CET January 2023 session at AIIMS, Patna:
| Course | Subject/Specialty | Total Number of Seats | UR | OBC | SC | ST | EWS |
| MD | Anaesthesiology | 18 | 8 | 5 | 3 | 1 | 1 |
| MD | Anatomy | 5 | 3 | 1 | 0 | 1 | 0 |
| MD | Biochemistry | 9 | 4 | 3 | 2 | 0 | 0 |
| MD | Community Medicine & Family Medicine | 8 | 3 | 2 | 1 | 0 | 2 |
| MD | Dermatology | 1 | 0 | 0 | 1 | 0 | 0 |
| MS | ENT | 2 | 1 | 0 | 0 | 1 | 0 |
| MD | Emergency Medicine | 7 | 2 | 2 | 2 | 0 | 1 |
| MD | FMT (Forensic Medicine & Toxicology) | 4 | 2 | 1 | 0 | 0 | 1 |
| MD | Medicine | 6 | 5 | 1 | 0 | 0 | 0 |
| MD | Microbiology | 3 | 1 | 1 | 1 | 0 | 0 |
| MD | OBG (Obstetrics & Gynaecology) | 5 | 1 | 1 | 0 | 2 | 1 |
| MD | Ophthalmology | 4 | 1 | 1 | 1 | 0 | 1 |
| MS | Orthopaedics | 5 | 2 | 2 | 1 | 0 | 0 |
| MD | Pediatrics | 7 | 2 | 2 | 1 | 1 | 1 |
| MD | Pathology | 5 | 0 | 2 | 1 | 1 | 1 |
| MD | Pharmacology | 3 | 3 | 0 | 0 | 0 | 0 |
| MD | Physiology | 7 | 4 | 2 | 1 | 0 | 0 |
| MD | PMR | 2 | 0 | 1 | 1 | 0 | 0 |
| MD | Psychiatry | 4 | 2 | 1 | 0 | 0 | 1 |
| MD | Radiodiagnosis | 4 | 1 | 1 | 1 | 1 | 0 |
| MD | Radiotherapy | 2 | 0 | 2 | 0 | 0 | 0 |
| MS | Surgery | 5 | 2 | 1 | 1 | 0 | 1 |
| MCh | Pediatric Surgery (MCh 6 Years) | 3 | 3 | 0 | 0 | 0 | 0 |
Table 6: Tentative seat distribution for INI-CET January 2023 session at AIIMS, Raipur:
| Course | Subject/Specialty | Total Number of seats | UR | OBC | SC | ST | EWS |
| MD | Anaesthesiology | 13 | 4 | 4 | 2 | 1 | 2 |
| MD | Anatomy | 3 | 2 | 1 | 0 | 0 | 0 |
| MD | Biochemistry | 4 | 1 | 1 | 1 | 0 | 1 |
| MD | Community Medicine | 8 | 3 | 2 | 1 | 1 | 1 |
| MD | Dermatology | 2 | 1 | 0 | 1 | 0 | 0 |
| MD | Emergency Medicine | 8 | 3 | 2 | 1 | 1 | 1 |
| MS | ENT | 5 | 2 | 2 | 1 | 0 | 0 |
| MD | Forensic Medicine & Toxicology | 2 | 1 | 0 | 0 | 0 | 1 |
| MD | General Medicine | 9 | 4 | 3 | 1 | 0 | 1 |
| MS | General Surgery | 8 | 3 | 3 | 1 | 0 | 1 |
| MD | Microbiology | 5 | 2 | 2 | 1 | 0 | 0 |
| MD | Nuclear Medicine | 1 | 0 | 0 | 0 | 1 | 0 |
| MD | Obstetrics & Gynaecology | 7 | 2 | 1 | 2 | 0 | 2 |
| MD | Ophthalmology | 8 | 4 | 2 | 1 | 1 | 0 |
| MS | Orthopaedics | 5 | 2 | 1 | 1 | 0 | 1 |
| MD | Pediatrics | 7 | 3 | 1 | 1 | 1 | 1 |
| MD | Pathology | 8 | 4 | 2 | 2 | 0 | 0 |
| MD | Pharmacology | 3 | 2 | 1 | 0 | 0 | 0 |
| MD | Physical Medicine & Rehabilitation | 2 | 0 | 1 | 1 | 0 | 0 |
| MD | Physiology | 2 | 0 | 1 | 0 | 0 | 1 |
| MD | Psychiatry | 4 | 1 | 1 | 1 | 1 | 0 |
| MD | Radiodiagnosis | 4 | 1 | 2 | 1 | 0 | 0 |
| MD | Radiotherapy | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Transfusion Medicine | 4 | 3 | 1 | 0 | 0 | 0 |
| MDS | Oral & Maxillofacial Surgery (MDS) | 1 | 1 | 0 | 0 | 0 | 0 |
| MDS | Pediatric and Preventive Dentistry (MDS) | 1 | 0 | 1 | 0 | 0 | 0 |
Table 7: Tentative seat distribution for INI-CET January 2023 session at AIIMS, Rishikesh:
| Course | Subject/Specialty | Total Number of Seats | UR | OBC | SC | ST | EWS |
| MD | Anaesthesiology | 7 | 3 | 2 | 1 | 0 | 1 |
| MD | Anatomy | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Biochemistry | 4 | 2 | 0 | 0 | 1 | 1 |
| MD | Community & Family Medicine | 3 | 2 | 1 | 0 | 0 | 0 |
| MD | Dermatology & Venerology | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Emergency Medicine | 3 | 2 | 0 | 1 | 0 | 0 |
| MS | ENT | 3 | 2 | 1 | 0 | 0 | 0 |
| MD | Forensic Medicine & Toxicology | 2 | 1 | 0 | 0 | 0 | 1 |
| MD | General Medicine | 4 | 3 | 1 | 0 | 0 | 0 |
| MD | Geriatric Medicine | 1 | 0 | 1 | 0 | 0 | 0 |
| MS | General Surgery | 3 | 1 | 1 | 0 | 0 | 1 |
| MD | Microbiology | 2 | 1 | 0 | 0 | 0 | 1 |
| MD | Nuclear Medicine | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Obstetrics & Gynaecology | 8 | 4 | 2 | 1 | 1 | 0 |
| MD | Ophthalmology | 6 | 4 | 1 | 1 | 0 | 0 |
| MS | Orthopaedics | 3 | 1 | 1 | 1 | 0 | 0 |
| MD | Pediatrics | 3 | 1 | 1 | 1 | 0 | 0 |
| MD | Pathology | 5 | 3 | 1 | 1 | 0 | 0 |
| MD | Pharmacology | 2 | 1 | 0 | 0 | 0 | 1 |
| MD | Physical Medicine & Rehabilitation | 2 | 1 | 0 | 1 | 0 | 0 |
| MD | Physiology | 3 | 2 | 0 | 0 | 0 | 1 |
| MD | Psychiatry | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Radiation Oncology | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Radiodiagnosis | 4 | 2 | 1 | 0 | 0 | 1 |
| MD | Respiratory Medicine | 3 | 2 | 1 | 0 | 0 | 0 |
| MD | Transfusion Medicine | 3 | 2 | 1 | 0 | 0 | 0 |
| MDS | Periodontics (MDS) | 1 | 1 | 0 | 0 | 0 | 0 |
| MDS | Oral & Maxillofacial Surgery (MDS) | 1 | 1 | 0 | 0 | 0 | 0 |
| MCH 6 Years | Pediatric Surgery (MCH 6 Years) | 2 | 2 | 0 | 0 | 0 | 0 |
| MCh | Plastic, Reconstructive & Burns Surgery (M.CH. 6 Years) | 2 | 2 | 0 | 0 | 0 | 0 |
| MCh | Neurosurgery (MCH 6 yrs) | 1 | 1 | 0 | 0 | 0 | 0 |
Table 8: Tentative seat distribution for INI-CET January 2023 session at AIIMS, Nagpur:
| Course | Subject/Specialty | Total Number of Seats | UR | OBC | SC | ST | EWS |
| MD | Anaesthesiology | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Anatomy | 1 | 0 | 0 | 0 | 0 | 1 |
| MD | Biochemistry | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Community Medicine | 3 | 1 | 2 | 0 | 0 | 0 |
| MD | Dermatology | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Forensic Medicine & Toxicology | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | General Medicine | 3 | 0 | 2 | 0 | 0 | 1 |
| MS | General Surgery | 3 | 0 | 1 | 1 | 1 | 0 |
| MD | Microbiology | 3 | 1 | 1 | 1 | 0 | 0 |
| MD | Obstetrics & Gynaecology | 3 | 1 | 1 | 1 | 0 | 0 |
| MD | Ophthalmology | 1 | 1 | 0 | 0 | 0 | 0 |
| MS | Orthopaedics | 1 | 1 | 0 | 0 | 0 | 0 |
| MS | Otorhinolaryngology | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Pediatrics | 3 | 0 | 1 | 0 | 1 | 1 |
| MD | Pathology | 3 | 0 | 1 | 1 | 1 | 0 |
| MD | Pharmacology | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Physiology | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Psychiatry | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Radiodiagnosis | 1 | 1 | 0 | 0 | 0 | 0 |
| MDS | Conservative Dentistry & Endodontics (MDS) | 0
|
0 | 0 | 0 | 0 | 0 |
Table 9: Tentative seat distribution for INI-CET January 2023 session at AIIMS, Bibinagar:
| Course | Subject/Specialty | Total Number of Seats | UR | OBC | SC | ST | EWS |
| MD | Anatomy | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Anaesthesiology | 2 | 2 | 0 | 0 | 0 | 0 |
| MD | Biochemistry | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Community Medicine & Family Medicine | 2 | 1 | 0 | 1 | 0 | 0 |
| MD | FMT | 1 | 0 | 1 | 0 | 0 | 0 |
| MD | General Medicine | 2 | 1 | 0 | 0 | 0 | 1 |
| MS | General Surgery | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Microbiology | 2 | 1 | 0 | 0 | 1 | 0 |
| MD | Obstetrics & Gynaecology | 2 | 0 | 1 | 1 | 0 | 0 |
| MS | Orthopaedics | 2 | 2 | 0 | 0 | 0 | 0 |
| MD | Peediatrics | 2 | 0 | 1 | 1 | 0 | 0 |
| MD | Pathology | 2 | 1 | 0 | 0 | 0 | 1 |
Table 10: Tentative seat distribution for INI-CET January 2023 session at AIIMS, Bathinda:
| Course | Subject/Specialty | Total Number of Seats | UR | OBC | SC | ST | EWS |
| MD | Anatomy | 1 | 0 | 0 | 1 | 0 | 0 |
| MS | General Surgery | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Microbiology | 2 | 1 | 0 | 0 | 1 | 0 |
| MD | Ophthalmology | 1 | 0 | 0 | 0 | 1 | 0 |
| MD | Physiology | 1 | 0 | 0 | 1 | 0 | 0 |
| MD | Psychiatry | 1 | 0 | 1 | 0 | 0 | 0 |
Table 11: Tentative seat distribution for INI-CET January 2023 session at AIIMS, Deoghar:
| Course | Subject/Specialty | Total Number of Seats | UR | OBC | SC | ST | EWS |
| MD | Biochemistry | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Community Medicine & Family Medicine | 1 | 1 | 0 | 0 | 0 | 0 |
| MS | General Surgery | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Microbiology | 1 | 0 | 1 | 0 | 0 | 0 |
| MD | Pharmacology | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Physiology | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Anaesthesiology | 1 | 0 | 0 | 1 | 0 | 0 |
| MD | Anatomy | 1 | 0 | 1 | 0 | 0 | 0 |
| MD | FMT | 1 | 1 | 0 | 0 | 0 | 0 |
| MS | Orthopaedics | 1 | 0 | 0 | 0 | 0 | 1 |
| MD | Pathology | 1 | 1 | 0 | 0 | 0 | 0 |
Table 12: Tentative seat distribution for INI-CET January 2023 session at AIIMS, Mangalagiri:
| Course | Subject/Specialty | Total Number of Seats | UR | OBC | SC | ST | EWS |
| MD | Anaesthesiology | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Anatomy | 2 | 0 | 0 | 1 | 0 | 1 |
| MD | Community & Family Medicine | 2 | 1 | 0 | 0 | 1 | 0 |
| MS | ENT | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | General Medicine | 1 | 1 | 0 | 0 | 0 | 0 |
| MS | General Surgery | 2 | 1 | 0 | 1 | 0 | 0 |
| MD | OBG | 2 | 0 | 1 | 0 | 0 | 1 |
| MS | Orthopaedics | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Pediatrics | 2 | 1 | 0 | 1 | 0 | 0 |
| MD | Pharmacology | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Physiology | 1 | 0 | 1 | 0 | 0 | 0 |
| MD | Psychiatry | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Radiodiagnosis | 2 | 1 | 1 | 0 | 0 | 0 |
Table 13: Tentative seat distribution for INI-CET January 2023 session at AIIMS, Raebareli:
| Course | Subject/Specialty | Total Number of Seats | UR | OBC | SC | ST | EWS |
| MD | Anaesthesiology | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Anatomy | 2 | 0 | 0 | 1 | 0 | 1 |
| MD | Community & Family Medicine | 2 | 1 | 0 | 0 | 1 | 0 |
| MS | ENT | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | General Medicine | 1 | 1 | 0 | 0 | 0 | 0 |
| MS | General Surgery | 2 | 1 | 0 | 1 | 0 | 0 |
| MD | OBG | 2 | 0 | 1 | 0 | 0 | 1 |
| MS | Orthopaedics | 2 | 1 | 1 | 0 | 0 | 0 |
| MD | Pediatrics | 2 | 1 | 0 | 1 | 0 | 0 |
| MD | Pharmacology | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Physiology | 1 | 0 | 1 | 0 | 0 | 0 |
| MD | Psychiatry | 1 | 1 | 0 | 0 | 0 | 0 |
| MD | Radiodiagnosis | 2 | 1 | 1 | 0 | 0 | 0 |
Last-Minute Tips for INI-CET Exam:
- Candidates must carry all the asked documents such as INI-CET admit card, passport size photograph, valid photo ID proof, and a copy of MCI registration certificate with them on the exam day.
- Reverify all your documents before coming to the exam hall.
- Candidates are advised to go through all the guidelines issued by AIIMS for the examination.
- Candidates must reach the INI-CET exam center before time to avoid any chaos.
- Avoid Stress and be confident.
- Eat healthy and sleep well.
- Time management is a must before and during the exam.
To get conceptual clarity on the MBBS courses online, click here
The National Medical Commission (Undergraduate Medical Education Board) has issued new guidelines and the academic calendar for MBBS 2022-2023 batch on 12th Oct 2022.
As per the new NMC guidelines, the classes for the first-year MBBS batch will start on 15th Nov 2022.
Academic Calendar for the 2022-2023 MBBS Batch
According to the new NMC guidelines, there is a change in the academic calendar of MBBS 2022-2023. However, the duration of the MBBS course is the same i.e., 5.5 years including a one-year rotational internship.
| Professional Year | Time Frame | Subjects | Months(Teaching + Exam + Results) |
| 1st | 15th Nov’22 to 15th Dec’23 | Anatomy, Physiology, Biochemistry | 13 months |
| 2nd | 16th Dec’23 to 15th Jan’25 | Pathology, Microbiology, and Pharmacology | 13 months |
| 3rd (III-part-1) | 16th Jan’25 to 30th Nov’25 | Forensic Medicine and Toxicology, Community Medicine/PSM | 10.5 months |
| 4th (III-part-2) | Dec’25 to May’27 | General Surgery, General Medicine, Pediatrics, Obstetrics & Gynecology, ENT, Ophthalmology |
17.5 months |
| Internship | 1st Jun’27 to 31st May’28 | As per the CRMI 2021 Regulations | 12 months |
| PG | 1st Jul ‘28 |
For the academic year 2022-2023, the one-year compulsory rotational internship will start from the 1st June 2027 and end on 31st May 2028, as per the CRMI 2021 regulations.
The following guidelines have been issued by the NMC for the 2022-23 MBBS batch:
- The MBBS batch will commence on 15th Nov 2022.
- The college vacations and examination schedules may be notified as per the affiliated universities of the respective colleges.
Other board guidelines are as follows:
- Regarding Electives – 2 blocks of 15 days each are to be adjusted by the colleges for
- Pre/para-clinical branches
- Clinical branches
- In the 2022-2023 academic batch, the supplementary exams will be conducted with a gap of 1 month from the regular exams and the results will be declared within 15 days.
- There shall be no supplementary MBBS batches.
- The remaining rules and regulations shall remain the same as per the GMER (Graduate Medical Education Regulations) 1997. You can visit the site for GMER 1997 details: https://www.nmc.org.in/rules-regulations/graduate-medical-education-regulations-1997/
- The Yoga and Family Adoption Program through village outreach shall continue for the 2021-2022 MBBS Batch.
Along with the changes in the curriculum and the guidelines mentioned above, a few more notifications have been issued by the NMC from the 2022 batch:
- The NMC has created an Anti-Ragging Committee and Dr. Aruna V. Vanikar, President, UGMEB has been appointed as the chairperson of the committee.
- In the NMC notification stated on 4 Oct 2022, the implementation of HMIS (Hospital Management Information System) is mandated in all medical colleges.
- The NEET UG counselling link is active from 11th Oct 2022 on the MCC official website: https://mcc.nic.in.
Click here to read about the NMC NExT Exam update 2023 including the guidelines, complete structure, exam dates and more.
Christian Medical College (CMC), Vellore is a private medical college, hospital, and research institute. CMC is one of the best private medical colleges in India. In and around Vellore, Tamil Nadu, India, this institute has a network of primary, secondary, and tertiary care hospitals. Dr. Ida Scudder is the founder of CMC Vellore. The college is affiliated with the Tamil Nadu Dr. M.G.R. Medical University, Chennai. CMC, Vellore is approved by NMC (National Medical Commission). It is ranked as one of the top medical colleges in India. The institution offers admission to various disciplines of sciences: medical science, nursing, allied health sciences, some other master’s and doctoral programs, and post-graduate engineering programs.
The college offers admission to various programs including:
- Undergraduate medical course (MBBS)
- Medical postgraduate courses (diploma, degree, and higher speciality courses)
- Certification courses
- Postdoctoral fellowship courses
- Distance education program
- Undergraduate nursing program
- Nursing postgraduate courses (diploma, degree, and fellowships)
- Allied health sciences degree courses
- MBA in hospital and health systems management (HHSM)
- MS Bioengineering
- Tech. Clinical Engineering
- D. Medical Sciences
MBBS in CMC Vellore
MBBS is a four-and-a-half-year course followed by one year compulsory rotating residential internship. In CMC, Vellore, the MBBS course comes under the group A category. As per the CBME curriculum, the undergraduate course in medicine comprises three phases.
Three phases in MBBS Curriculum
| Phases in MBBS Curriculum | Duration | Subjects Included |
| 1 (Pre-Clinical Phase) | 13 months | Basic Sciences, Anatomy, Physiology, Biochemistry, Introduction to Community Medicine, Humanities, and Professional Development |
| 2 (Para-Clinical Phase) | 12 months | Pharmacology, Pathology, and Microbiology |
| 3 (Clinical Phase) | Part 1: 13 months
Part 2: 13 months |
Forensic Medicine, Community Medicine, Ophthalmology, and Otorhinolaryngology.
Medicine and Allied Specialties, Surgery & Allied Specialties, Child Health, and Obstetrics & Gynecology. |
Block postings and Internship at CMC Vellore
As per the guidelines of the National Medical Commission,
- Along with regular classes, medical students also have to undergo block postings after phase 1 of their MBBS course at community health centers, mission hospitals, and secondary care centers.
- A medical student also has to compulsorily complete the rotational internship for 12 months. They are posted in the discipline of community health, medicine, surgery, obstetrics & gynecology, orthopaedics, emergency medicine, and short elective subjects.
- At CMC, Vellore, the students are allocated community health centers, mission hospitals, and secondary care centers for internships.
Admission procedure
Admission to the MBBS undergraduate course in CMC, Vellore solely depends on the NEET-UG score. An aspirant to get admission at CMC needs to qualify and crack the NEET-UG (National Eligibility cum Entrance Test) examination with a good score.
Eligibility to get admission at Christian Medical College
- Candidate must have completed 10+2 higher secondary schooling or equivalent examination, and the last two years of education must include Physics, Chemistry, and Biology/Biotechnology as major subjects with English from the Tamil Nadu State board or any other equivalent examination board.
- Candidates must have attained a minimum of 50% marks in all the subjects, Physics, Chemistry, Biology/Biotechnology, and English individually for the general category, and a minimum of 40% aggregate for BC, MBC, SC/ST candidates is required in a single attempt. The criteria mentioned are subject to change as per the state & university guidelines.
- At the time of admission, a candidate must have completed 17 years of age or should complete the mentioned on or before 31st December of the said year.
NEET-UG Exam Pattern for admission to MBBS at CMC Vellore
The NEET-UG exam is conducted by National Testing Agency (NTA) once a year. The following are some important points to keep in mind:
| Particulars | Description |
| Exam Mode | Offline (pen & paper based) |
| Type of Examination | Multiple choice questions |
| The total number of questions | 200 questions (180 MCQs must be answered) |
| NEET total marks | 720 marks |
| Marking scheme | +4 for each correct answer and -1 for every incorrect answer |
| Total duration | 3hrs 20 mins |
| Languages | The exam is conducted in 13 different languages, namely, English, Hindi, Assamese, Bengali, Gujarati, Malayalam, Kannada, Marathi, Odia, Tamil, Telugu, Urdu, and Punjabi |
NEET Exam Section-wise Distribution:
In all 4 Subject sections, Physics, Chemistry, Biology, and Zoology, there are two sections, section A comprises 35 questions and section B comprises 15 questions out of which 10 are to be answered. Each question carries 4 marks.
Number of Seats for 2022-2023 at CMC, Vellore
The total number of MBBS candidate seats is 100 and the seat distribution is as follows:
- All India open category: 16 seats
a. One candidate is selected by Govt. of India under the ‘Central Pool Scheme’.
b. 20% i.e., 3 seats are reserved for the SC/ST candidates. - Minority Network Category & CMC, Vellore staff quota: 84 Seats
Steps to get admission into CMC Vellore
- Fill out the application form for an undergraduate course from the CMC, Vellore official site.
- Provide your NEET application form details.
- Submission of the receipts of the certification forms from Minority Network Organizations (if applicable).
- Apply to the Tamil Nadu Selection Committee for the counseling process in the relevant category.
- The selection is based on the NEET-UG score and candidates are required to fill the NEET-UG score and rank on the CMC, Vellore admission site.
- Submission of the Arno & rank of TN Management Quota.
- Be updated with the release of the merit list.
- Counseling by Tamil Nadu Selection Committee, DME, Chennai.
All these steps are to be done in the stipulated period as provided by the college. So, be updated.
Admission Process after Counseling at CMC, Vellore
- After the counseling procedure, the candidate is required to register for the course by paying the tuition fees and completing other formalities, and submitting original certificates.
- The admission confirmation is approved by Tamil Nadu Dr. M.G.R. Medical University. Until the approval, admission continues to be provisional.
- After the confirmation of the MBBS admission at CMC, Vellore, a candidate needs to submit their original required documents at the university campus.
- All the candidates getting admission to CMC, Vellore need to undergo a medical fitness check-up and the admission gets confirmed only after the medical fitness clearance by the Medical Board, CMC, Vellore.
MBBS Course Fee at CMC, Vellore
The fees to be paid at the time of registration for admissions to the MBBS course at CMC, Vellore is mentioned in the table below:
| Particulars | Fees (in rupees) |
| Tuition fees | 3,000 |
| One-time College fee at Admission | 10,300 |
| Other Annual Fee | 25,105 |
| One-time payment to the University | 14,425 |
| Total | 52,830 |
*The course fee may change in the coming years depending upon the University rules and regulations.
MBBS Cut-off at CMC, Vellore
Based upon the analysis of the previous years’ cut-offs, the estimated NEET-UG cut-off marks for the MBBS course for admission at CMC, Vellore are mentioned below:
| Category | Estimated Cut off Score |
| General | 600 |
| Minority | 380 |
| Institutional/Staff | 500 |
| SC/ST | 520 |
To get the conceptual clarity on the MBBS courses online, click here.
Medical Postgraduate Courses at CMC, Vellore
In CMC, Vellore Admission to PG Degree, Diploma, PG diploma courses, and fellowship courses come under the Group B category. Admission to the MD/MS courses is done based on the NEET-PG score. All the students need to get into the NEET-PG merit list for admission to the PG courses with the required cut-off score.
PG Courses and Number of Seats
The Christian Medical College offers admission to various post-graduate specialization courses.
- The CMC Vellore provides admission to MD courses for various subjects along with the number of seats mentioned below:
| MD Specialization Courses | Number of Seats |
| Anaesthesiology | 33 |
| Anatomy | 4 |
| Biochemistry | 2 |
| Community Medicine | 6 |
| Dermatology Venerol & Lep. | 5 |
| Emergency Medicine | 3 |
| Family Medicine | 2 |
| Geriatrics | 3 |
| General Medicine | 16 |
| Microbiology | 4 |
| Nuclear Medicine | 2 |
| Pediatrics | 20 |
| Pathology | 8 |
| Pharmacology | 2 |
| Physiology | 4 |
| Physical Medicine & Rehabilitation | 4 |
| Psychiatry | 12 |
| Radiodiagnosis | 12 |
| Radiation Oncology | 8 |
| Respiratory Medicine | 4 |
| Transfusion Medicine | 3 |
- The CMC Vellore provides admission to MS courses for various subjects along with the number of seats mentioned below:
| MS specialization Courses | Number of Seats |
| Otorhinolaryngology | 8 |
| General Surgery | 10 |
| Obstetrics & Gynecology | 17 |
| Ophthalmology | 9 |
| Orthopaedics | 12 |
Service Obligation at CMC, Vellore
- The service obligation of 3 years is mandated for all the MS/MD candidates, except for the clinical specialties (General merit category).
- Candidates admitted to the clinical specialties under the general merit category have a service obligation of 1 year.
- Candidates admitted to the pre-and para-clinical specialties under the general merit category, have no service obligation.
- For diploma courses, the service obligation period is a minimum of 2 years whereas, general merit candidates are exempted from the same.
- After the course completion, the service obligation is served at the CMC, Vellore or any of the associated mission hospitals.
Facilities available for the medical PG trainees
- Stipend
- Accommodation
- Research activity of each department
- Medical records department
- Recreation
- Staff/student health clinic
Fee Structure for the Postgraduate Medical Courses at CMC, Vellore
The fees to be paid at the time of registration for admissions to the Medical PG courses (MD/MS) at CMC are mentioned in the table below:
| Particulars | 2 yr Post Diploma Degree (in rupees) | 3 yr PG Degree (in rupees) |
| Tuition fees | 800 | 1200 |
| One-time admission fees | 1200 | 30,000 |
| University fees | 1,35,610 | 1,35,610 |
| Others | 17,600 | 19,600 |
| Total | 1,74,010 | 1,86,410 |
*The course fee may change in the coming years depending upon the University rules and regulations.
NEET-PG Cut-off Score for MS/MD admission to CMC, Vellore
Based upon the analysis of the previous years’ cut-offs, the estimated cut-off marks for the medical PG specialization courses for admission at CMC, Vellore are mentioned below:
| Specialization | Estimated Cut-off Score |
| Anesthesiology | 400 |
| Anatomy | 460 |
| Biochemistry | 430 |
| Community Medicine | 500 |
| Dip. In Clinical Pathology | 480 |
| Dermatology Venerol & Lep. | 540 |
| Emergency Medicine | 500 |
| Family Medicine | 450 |
| Geriatrics | 380 |
| General Surgery | 460 |
| General Medicine | 590 |
| Microbiology | 450 |
| Neurosurgery | 500 |
| Nuclear Medicine | 500 |
| Obstetrics & Gynecology | 380 |
| Ophthalmology | 400 |
| Orthopedics | 450 |
| Pediatrics | 440 |
| Pathology | 450 |
| Pharmacology | 600 |
| Physiology | 480 |
| Physical Medicine & Rehabilitation | 450 |
| Psychiatry | 360 |
| Radiodiagnosis | 450 |
| Radiation Oncology | 450 |
| Respiratory Medicine | 490 |
| Transfusion Medicine | 600 |
Certificate courses after MBBS
The certificate courses offered by the CMC Vellore for the MBBS graduates are mentioned below:
| Course Name | Duration | Number of Seats |
| Accident & Emergency Medicine | 2 years | 10 |
| Neonatology | 1 year | 1 |
| Palliative Medicine | 1 year | 2 |
| Acute Care Pediatrics | 1 year | 1 |
- CMC, Vellore also provides admission to various higher specialty and Postdoctoral diploma courses and allied health sciences courses.
- After completing MBBS, a medico can also pursue M.Sc. Epidemiology and Master of Public Health Administration.
CMC, Vellore Hostel Fees and Facility
- Hostel Facility for MBBS Students: MBBS students live in the campus hostels. The Bagayam campus of the CMC, Vellore has girls’ and boys’ hostels. The girls’ hostel is named as ‘Paradise on Earth’, while the boys’ hostel is named as ‘Mansion of the Gods’. Boys are required to submit the hostel charges (Deposits and advance) of10,000/- and girls Rs.8,000/-. The approximate living expenses per month for the hostel are Rs.6,000/- for boys and girls.
- Hostel facility for other courses: The women’s hostel and men’s hostel for the students of allied health courses are named as the ‘Fitch Hostel’ and the ‘Dorothy Joske Hostel’. The ‘Modale International Hostel’ is allocated for the elective course students/visitor observer students from overseas. The hostel and its charges vary as per the student’s course.
All the hostels are well equipped with all the necessities of a student and other facilities such as a Hostel Chapel, recreation room, gymnasium, library, dance room, music room, prayer room, mini kitchen, TV/Projector room. The food facility with vegetarian and non-vegetarian food is also available for all the residents.
How does DigiNerve help a medico?
DigiNerve is an EdTech initiative by Jaypee Brothers, a pioneer and market leader in health science publishing with a legacy spanning over 5 decades. It provides top-notch medical content to enhance conceptual clarity, clinical skills, and ace exams.
In terms of the calibre of the courses, the variety of subjects, the Gold Standard faculty, and the user-friendly interface, DigiNerve is unmatched.
- DigiNerve provides best online courses for MBBS subjects designed by eminent faculty as per CBME Curriculum and NEET Exam, such as
| MBBS Online Courses | Course Faculty |
| Community Medicine for UnderGrads | Dr. Bratati Banerjee |
| Forensics Medicine and Toxicology for UnderGrads | Dr. Gautam Biswas |
| Medicine for UnderGrads | Dr. Archith Boloor |
| Microbiology for UnderGrads | Dr. Apurba S Sastry, Dr. Sandhya Bhat, Dr. Deepashree R |
| OBGYN for UnderGrads | Dr. K Srinivas |
| Ophthalmology for UnderGrads | Dr. Parul Ichhpujani, Dr. Talvir Sidhu |
| Orthopaedics for UnderGrads | Dr. Vivek Pandey |
| Pathology for UnderGrads | Prof. Harsh Mohan, Prof. Ramadas Nayak, Dr. Debasis Gochhait |
| Pediatrics for UnderGrads | Dr. Santoah T Soans, Dr. Soundarya Mahalingam |
| Pharmacology for UnderGrads | Dr Sandeep Kaushal, Dr. Nirmal George |
| Surgery for UnderGrads | Dr. Sriram Bhat M |
- Apart from the MBBS and MD courses, DigiNerve brings the professional courses ‘Ultrasound in OBGYN Made Easy’ and ‘Basics of Infertility and IUI Made Easy’ by the top faculty Dr. Chaitanya Nagori and Dr. Sonal Panchal. After completion of the course, the candidates will earn a course completion certificate from Ian Donald Inter-University School of Medical Ultrasound.
- An Exam preparation course ‘Cracking MRCP Part 1’ by Dr. Gurpreet Singh Wander and Dr. Archith Boloor, helps a medico with their preparation to crack the MRCP exam. Cracking MRCP Part 1 course is based on the curriculum devised by The Royal College of Physicians (RCP). The course has 15 online modules covering major specialties such as Clinical Sciences, Cardiology, Gastroenterology, etc. The course includes video lectures, e-chapters, 2500+ BOF questions, mock exams, and most of all high-quality notes.
FAQs
-
How many marks are required in NEET for MBBS in CMC Vellore?
Ans: The estimated cut off score for admission to CMC, Vellore is around 600+ in the NEET Examination for general category. For the OBC/SC/ST & Minority groups, the estimated cut-off score is around 500 marks. For sponsored & management quota students, the cut-off range is comparatively lower.
-
Is CMC Vellore a deemed university?
Ans: No, CMC Vellore is not a deemed University. It is a private college, affiliated with Tamil Nadu Dr. M.G.R. Medical University, Chennai run by the Christian community.
-
Is CMC good for MBBS?
Ans: CMC Vellore is ranked 3rd as per NIRF ranking 2022 after AIIMS, Delhi, and PGIMER, Chandigarh. It is one of the best medical colleges in India.
Most students think that medical education is only about clearing the entrance exam and getting admission to MBBS. However, the reality is way different than this perception. Clearing the exam isn’t the final step, rather, is the beginning of the life of a medical student. A medical degree is considered one of the toughest degrees in the world. For a student, it’s definitely more work because of the unlimited workload and the time limit, which means a lot less sleep and a lot more stress.
Top Struggles of MBBS Students are:
- Adjusting with peers: Medical colleges are responsible for ensuring that graduates are knowledgeable, skilful, and professional to meet society’s expectations. Due to this, students have to prepare themselves for the vast syllabus while also adjusting with peers. There is huge peer pressure on medical students when it comes to adjusting themselves in the new environment due to high level of competition.
- Wow! You are smart, you should be a doctor: Medical might not be the hardest choice for aspirants but the journey is indeed very hard. Students put in all the efforts, and energy to enter the clinical world; the world that includes a lot of hard work, sleepless nights, countless hours of study, and whatnot. However, there are many students who give their 100 percent just to satisfy that One Big Dream of their family and relatives, at the cost of their happiness.
- Do you have a social life? When it comes to a medical student’s social life, the status is quite complicated. Students get trapped with books, assignments and practices, etc. that they can’t focus much on their social life. Although medicine is a very social course and being a healthcare professional, students must know how to deal with people. To take time out for social activities, students need to maintain a schedule that allows them to manage it all.
- Start the day and end the day with medicine: – The primary motivation is to enjoy studying. Exhaustion due to continuous studies can make medical college seem like a burden. So students must divert their attention from studies a bit and focus on “personal development.” This involves honing talents that fall outside the purview of academic study yet are nevertheless crucial for a doctor. For instance, participating in music or theatre can help students get used to performing or interacting in front of a large audience. This also helps them to confidently address and speak at a conference or simply to a group of their coworkers. There is a balance that needs to be achieved between working and enjoying life.
- You have to memorize so many new drugs, that your brain might explode: The most problematic situation that students face is that they need to cram names of thousands of new drugs and various syndromes, which is confusing. Also since these drugs are vast along with their own different characteristics, it is easy to forget a few. This is not the end, memorizing drugs also includes knowing their purposes, advantages, and disadvantages, after effects, and what all changes can be possible, which also includes how they respond in every individual’s body.
Watch Video to learn the right way to approach Pharmacology in MBBS
- The unending workload: – It is a popular talking point that a medical student’s life in med college is endless. The reason behind this is that medical courses are the longest courses in the educational world. It nearly takes a decade to become a fully qualified doctor. The entire journey demands a lot of hard work, sleepless nights, and a huge number of complications. It is not easy to maintain patience throughout this period and often students lose themselves in the wheel of practicals, rounds, syllabus, and examinations.
- Finance: – Finance is a huge problem for a medical aspirant. How? Not all medical aspirants belong to financially stable families, and neither do all receive government scholarships. Many students dream to become a doctor, but again finances remain a challenge. Medical studies are considered one of the most expensive education all over the world. It is a vast and expensive course. If a student does not have an adequate amount of money, pursuing a medical degree can be challenging. If this problem arises while a student is pursuing the course, students should always have a backup option.
- Exams Breakdown: – Exams have always been a huge load. Even the thought of it is scary because the syllabus is so vast that sometimes the duration of preparation tends to seem less. There’s no doubt medical life is filled with competitors, which makes the exam period even more stressful. Skipping topics is another aspect that makes it stressful while spending more time on important topics. Additionally, lack of sleep, headaches, and stress can easily lead to breakdowns.
- A good night’s sleep is a wonder for you: – Back-to-back classes, practicals, and whatnot get tiresome for them. Most students have sleepless nights because of assignments, many even suffer from sleep deprivation or poor sleep quality which is common during the internship. Researchers have paid much attention to the critical function that sleep plays in preserving mental health, advanced learning, and overall welfare. From 1st year to the final year, medical students are particularly prone to sleep-related problems due to the huge syllabus. So it is very important for students to at least have 6 – 8 hours of sound sleep.
Life of Students in the 1st year of MBBS:
Medical College is nothing like high school; it is challenging not simply because there is so much knowledge to gain, but also because students get to learn new skills. Students mostly in their first year, try to understand what kind of studying technique works to cover the syllabus. The first year is all about learning, failing and again understanding where you were wrong and then starting again.
Life in college doesn’t resemble the medical drama– Grey’s Anatomy in reality. No one goes to the clinical rounds in the first year itself. In the first year, students study Biophysics, Anatomy, and Histology and prepare for tests most of the days.
In the first year, it’s not all about saving lives. The only life students can save is theirs, by fixing a decent study routine for themselves, figuring out how to adjust their studies and things they like doing beyond studying and getting sufficient rest.
Life of Students in the 2nd year of MBBS:
It’s the best time to retrospect and make a schedule that can help students manage studies, social life, and sleep. The one benefit students have in their 2nd year is that they get familiar with the environment, faculty, and course too, so it becomes a bit easy for them to communicate and discuss their problems in the class or with the faculty. It gets even easier to make a schedule that can be followed given that students get quite familiar with the frequency of classes, practicals, and tests.
Life of Students in the 3rd year of MBBS:
It is very much like climbing one more step and reaching one step near to the goal of becoming a Top Doc. Becoming more focused on studies and attending a lot of practicals are included in the 3rd year. It is time for students to get exposed to the practical technicalities of the field. Students become familiar with everyday struggles in 3rd year; they feel the sensation of being worn out, because of classes and clinical rounds. They need to have some sort of framework, whether it be a paper journal or a schedule reminder turned on on their mobile phones.
Life of Students in the 4th year of MBBS:
The significant cause of the pressure students face in the final year is due to the major subjects like Medicine, Surgery, Pediatrics, OBGYN, Orthopaedics, etc. which are highly important for NEET PG. They experience maximum stress when they start going for rounds. Medicine is a long-distance race, not a run. Regardless of whether students complete their last year, it isn’t the end. They still need to learn a lot more because now their real life as interns and saviours begin. It’s now time to put all the knowledge into application.
Get conceptual clarity in Medicine from Dr. Archith Boloor
Passing the final exam in MBBS is crucial to starting your career as a doctor. Students must focus on conceptual clarity to clear the final exams. Discipline and dedication are the keys to mastering the syllabus. Moreover, aspirants that are pursuing the MBBS program at any medical college must complete the internship. An internship is a term of learning, or, to put it in simple words, more practical work than theoretical training. The internship phase is where you put all of the theoretical information you’ve learned over the last four years into action.
You should have a proper plan if you are going to enrol yourself as a medical student, it is a long ride with lots of struggle, hard work, failures, and whatnot. The medical course is exceptionally vast due to the volume of material that needs to be learned along with both the basic scientific principles and the clinical abilities. Keeping in mind the surreal feeling that a doctor feels while saving someone’s life is something that can’t be put into words, and furthermore, the feeling of saving somebody’s life is simply inexplicable. Once your goal is set and you are ready for it, it is definitely going to be the best chapter of your life.
The specialised area of medicine known as ophthalmology is dedicated to eyes’ health. It covers the physiology, anatomy, and disorders that could impact the eyes. A professional doctor who deals with the prevention, diagnosis, and medical care of the eyes is an ophthalmologist. Ophthalmologists are trained in both surgical techniques and pharmacological therapies because this could involve both. M.D.s have the specialised training to offer the complete range of eye care, from performing intricate and delicate eye surgery to dispensing contact lenses and spectacles. Research into the causes and treatments for eye disorders and vision issues is another area of expertise for many eye doctors.
What does the PG Ophthalmology course focus on?
PG Ophthalmology programme lasts 3 years after students complete their MBBS degree. The course helps train students to treat eye conditions such as glaucoma, which damages the optic nerve and impairs vision, with the potential to result in blindness, iritis, which is an inflammation of the iris that may be caused by a systemic disease, chemical burns, orbital cellulite. Higher education and training in a variety of subspecialties are made available to enrolled students, from performing critical eye surgery to prescribing glasses and contact lenses. The course is well-structured for doctors to address any eye issues that may arise.
The course covers the fundamentals of ophthalmology as well as more complex topics such as disorders of the optical nerve system and the uvea and vitreoretinal tissues. According to analyses obtained through the use of medication, surgery, diet, and other therapies, doctors are taught how to cure eyes. The curriculum is developed to equip MD students with the knowledge and skills necessary to provide total eye care, including vision services, eye examinations, medical and surgical eye procedures, and the diagnosis and treatment of eye disorders and other visual difficulties.
DigiNerve’s Ophthalmology MD Course by Dr. N. Venkatesh Prajna
Dr. N. Venkatesh Prajna, the Editor-in-Chief of Ophthalmology MD has designed the course along with India’s 55 renowned faculty. Their collective expertise will help students remarkably to gain an in-depth knowledge of concepts. The course is designed from an academic, clinical, and surgical point of view. The in-video demonstration of various surgeries will give a whole new dimension to students’ postgraduate learning.
The Ophthalmology MD course is a thoughtfully compiled collection of topics from prominent ophthalmologists from across the nation. Around 400 topics that are significant from an academic, clinical, and surgical perspective are collected in the course. All of the course’s topics have been carefully chosen with consideration given to frequently asked questions and troublesome regions for postgraduate students to provide adequate knowledge.
This programme is one of the best PG Ophthalmology courses for students who are seeking to fare well in post-graduation. Components of the course appropriately match the requirement of students in the pre-operative workup, helping them to perform surgical skills and even handle post-operative difficulties. To meet all of the students’ learning needs, it promotes concept and approach-based learning.
Postgraduate students who are taking exams have a special section with an innovative examination corner. For frequently encountered ocular disorders, particular focus is placed on obtaining the proper clinical findings by following the proper case and history-taking procedures.
With the use of surgical videos combined with 3D animated sequences of every surgical step, practitioners could also develop clinical/surgical ophthalmic skills. The conceptual knowledge will take on a completely new dimension, thanks to the in-video display of the numerous surgeries being carried out.
To help students gain a full understanding of each topic and to prepare them for exams, the lectures are richly illustrated with clinical/surgical and radiological pictures, as well as flowcharts, tables, and boxes, wherever necessary. For many illnesses, recent evidence-based recommendations have been added to familiarise readers with recent developments in the field. The important diagnostic procedures and techniques have been covered in detail along with a drug chart for quick reference for the students with a special focus on drug dosages, adverse effects, and their indications/contraindications.
Table of Content – Ophthalmology MD by Dr. N. Venkatesh Prajna
Cataract
Lens
Anesthesia for Cataract Surgery
Preoperative Evaluation of Cataract Surgery
IOL Power Calculation
Ocular Viscosurgical Devices
Manual Extracapsular Cataract Extraction
Manual Small Incision Cataract Surgery – Basics
Manual Small Incision Cataract Surgery – Complications
Applications of Manual Small Incision Cataract Surgery
Secondary IOL Implantation Through Sclero-Corneal
Phacodynamics
Phacoemulsification Techniques
Cortical wash – Coaxial and Bimanual Irrigation Aspiration Techniques
Foldable IOLs, Loading and Implantation
Complications of Phacoemulsification
Applications of Phacoemulsification
Repositioning of IOL and IOL Exchange
Femto Laser Assisted Cataract Surgery
Lens Induced glaucoma
Instrument Sterilization
Cornea
Cornea Basics
Corneal Topography
Specular Microscopy
Confocal Microscopy
Bacterial Keratitis
Fungal Keratitis
Acanthamoeba Keratitis
Microsporidial Keratitis
Herpes Simplex Keratitis
Herpes Zoster Keratitis
Non Healing Keratitis/Non Healing Corneal Ulcers
Peripheral Ulcerative Keratitis I -General concepts
Corneal Ectasia
Pterygium
Limbal Stem Cell Deficiency
Ocular Cicatricial Pemphigoid
Chemical Injuries of the Eye
Limbal Epithelial Transplantation (SLET and CLET, Buccal)
Amniotic Membrane Transplantation
Keratoprosthesis
Management of Ocular Trauma
Contact Lens
Corneal retrieval and Eye banking
Penetrating keratoplasty
Therapeutic keratoplasty
Graft Rejection
Refractive Surgeries
Deep Anterior Lamellar Keratoplasty
Descemet Stripping Automated Endothelial Keratoplasty
Glaucoma
The Angle of Anterior Chamber
Aqueous Humour Dynamics
Tonometry
Central Corneal Thickness and Glaucoma
Gonioscopy
Pathogenesis of Glaucomatous Optic Neuropathy
Clinical Evaluation of the Optic Nerve Head
Optic Nerve Head Changes in Glaucoma
Interpreting Humphrey Visual Field Reports
Interpreting Octopus Perimetry Reports
Anterior Segment Imaging Imaging – Ultrasound Biomicroscopy and Anterior segment Optical Coherence Tomography
Optic Nerve Head Imaging/Role of OCT in Glaucoma
Classification of the Glaucomas
Ocular Hypertension
Primary Open Angle Glaucoma
Normal-Tension Glaucoma
Primary Angle Closure Disease
Pseudoexfoliation Glaucoma
Pigmentary Glaucoma
Lens Induced glaucoma
Uveitic Glaucoma
Neovascular Glaucoma
Glaucoma Associated with Ocular Trauma
Nanophthalmos and Other Secondary Angle Closure Glaucomas
Glaucoma after Vitreoretinal Surgery
Steroid Induced Glaucoma
Glaucoma following Penetrating Keratoplasty
Glaucoma Associated with Corneal Disorders
Classification and Early Diagnosis of Pediatric Glaucoma
Primary Congenital Glaucoma
Juvenile Open Angle Glaucoma
Glaucoma in Phacomatoses
Target Intra Ocular Pressure
Medical Management of Glaucoma
Newer Ocular Hypotensive Medications
Neuroprotection
Lasers in Glaucoma
Trabeculectomy
Glaucoma Drainage Devices
Non-Penetrating Deep Sclerectomy
Minimally Invasive Glaucoma Surgery
Cyclodestructive Procedures
Neuro-Ophthalmology
Practical Pearls in Neuro-ophthalmology
Neuro-ophthalmic Cases: Case Scenarios
Approach to Neuroimaging in Neuro-ophthalmology
Evaluation of a Case of Double Vision
Optic Neuritis
Optic Atrophy
Papilloedema
Myasthenia and Myopathies
Nystagmus-Evaluation
Double Vision A 10-step Assessment Plan
Myasthenia Gravis and its Mimickers
Neuro-Ophthalmic Examination: An Overview
MRI Making Sense of the Images
Neuroimaging for Ophthalmologists
Evaluation of a Pale Optic Disc
Optic Neuropathy
Pupil Pathways and Inference
Bilateral Ocular Motility Disorders – A Differential Diagnosis
An Approach to Swollen Optic Discs
Visual Fields in Neuro-ophthalmology
Ocular-Microbiology
Basic Microbiology
Antibiotics: Therapy and Testing
Molecular Diagnosis in Ocular Microbiology
Orbit
Anatomy of the Orbit
Lacrimal Apparatus
Imaging of the Orbit: Computed Tomography Scan
Orbital Decompression for Thyroid Orbitopathy
Proptosis- General Concepts
Orbital trauma- Considerations and principles
Orbital fractures and management
Orbit Infections
Fungal Infections of the Orbit
Parasitic Infections of the Orbit
Orbital Inflammations
Anophthalmic Socket
Contracted Socket
Benign tumors of the Orbit
Vascular Lesions of the Orbit
Reconstructive Socket Surgeries: Enucleation, Evisceration and Exenteration
Blepharoptosis: Evaluation and Management
Eyelid Retraction
Ectropion
Entropion
Esthetic Eyelid Surgery
Basics of Eyelid Reconstruction
Overview of Eyelid Reconstruction
Lacrimal Drainage System: Anatomy and Anomalies
Evaluation of the Lacrimal System
Congenital NasoLacrimal Duct Obstruction
Adult NasoLacrimal Duct Obstruction
Botulinum Toxin in Ophthalmology
Orbitotomy- Introduction
Lateral Orbitotomy
Orbitotomy – Other Approaches
Oncology
Pediatric Ophthalmology
Development of Visual System
Typical Development of Visual Milestones
Estimating Visual Acuity in a Child
Estimating Visual Acuity in Infant
Childhood Refractive Errors and Guidelines on Management
Lazy Eye
Red Eye in a Child and Vitamin A Deficiency
Syndromes with Ocular Manifestation
Low Vision (Visual Impairment)
Vision Assessment in Children with Low Vision
Low Vision Aids – Optical
Non Optical Aids and Rehabilitation
Headaches in Children
Ocular Causes of Headache
Retina
Macular Function Tests
Fundus Fluorescein Angiography
Indocyanine Green Angiography
Optical Coherence Tomography
OCT Angiography
USG + UBM
Fundus Autofluorescence and Multicolor Imaging
Retina
Anatomy, Physiology and Embryology of Vitreous
Evaluation of Retina and Vitreous
Diabetic Retinopathy
Hypertension and the Eye
Central Retinal Vein Occlusion
Branch Retinal Vein Occlusion
Age-related Macular Degeneration
Pachychoroid Spectrum Disease – Introduction and Pachychoroid Pigment Epitheliopathy
Central Serous Chorio-Retinopathy
Pachychoroid Neovasculopathy & Polypoidal Choroidal Vasculopathy (PCV)
Peripapillary Pachychoroid Syndrome & Focal Choroidal Excavation
Hereditary Macular Dystrophies
Macular Pathologies
Peripheral Retinal Degenerations
Retinopathy of Prematurity
Melanoma PG 1
Retinoblastoma
Paraneoplastic Retinopathy
Vascular Tumors of Retina and Choroid
Lasers in Retina
Intravitreal Injections
Rhegmatogenous Retinal Detachment
Non Rhegmatogenous Retinal Detachment
Posterior Segment Trauma
Systemic Diseases with Retinal Manifestations
Principles of Vitreoretinal Surgery
IOFB and its Management
Endophthalmitis
AI in Ophthalmology
Vitreoretinal Interface Diseases of the Macula – Epiretinal Membrane
Strabismus
Extra-Ocular Muscles & Orbital Fascia Applied Anatomy
Physiology of Extra Ocular Muscles
Binocular Single Vision
Strabismus – Classification & Etiology
Approach to a Comitant Deviation Patient
Diplopia
Hess Charting
Comitant Horizontal Strabismus: Esodeviation
Comitant Horizontal Strabismus: Exodeviation-
Vertical Deviation a. Approach to vertical deviations
Pattern Strabismus
Paretic Strabismus
Diagnosis and Management of Oculomotor Palsy
Diagnosis and Management of Trochlear Nerve Palsy
Diagnosis and Management of Abducent Nerve
Duanes Retraction Syndrome
Restrictive Strabismus
Browns Syndrome
Monocular Elevation Deficiency
Thyroid Related Strabismus
Congenital Fibrosis of Extra Ocular Muscles
Non-surgical Management of Strabismus
Surgical Management of Strabismus
Complications of Strabismus Surgery
Uvea
Uveal Tract
The SUN Classification & Terminologies of Uveitis
Systematic Work Up in Uveitis
Construction of Differential Diagnosis in Uveitis
Art of Ordering Lab Investigations in Uveitis
Immunosuppressives and New Biologicals
Management of Uveitic Cataracts
Ocular Tuberculosis
Viral Anterior Uveitis
Viral Uveitis
CMV – Posterior Uveitis
Leptospirosis & Syphilitic Uveitis
Ocular Toxoplasma
HIV and Opportunistic Infections Non Infectious Uveitis
Autoimmune Diseases and Uveitis
Sarcoidosis
VKH
Sympathetic Ophthalmia
The Masquerades
Refraction
Visual Acuity
Refractive Errors
Retinoscopy
Subjective Refraction
Accommodation and Convergence
Presbyopia Mechanism, Optical Correction and Surgical Procedures
Spectacle Lenses, Frames and Vertex Distance
Bifocals/Trifocals
Progressive Additional Lenses
Prisms
Contact Lenses
Colour Vision Contrast Sensitivity and Higher Order Aberrations
Aberrometer
Keratometry
Lensometer
Low Vision Aids
Examination Corner
How to Write a Theory Paper
How to Describe Clinical Finding in a Uveitis Case?
FAQs in a Uveitis Case
How to Describe Clinical Finding in a Cornea Case
How to Describe Clinical Finding in a Retina Case?
FAQs in a Fundus Case Pertaining to the Retinal Vessels
How to Describe Clinical Finding in a Glaucoma Case?
How to Describe Clinical Finding in a Orbit Case?
FAQs in a Orbit Case
How to Describe Management in Examinations
Investigations
OSCE Glaucoma
OSCE in Posterior Segment
OSCE in Neuro-ophthalmology
Ophthalmic Instruments
Best Way to Study Ophthalmology MD
- The postgraduate students should actively participate in lecture demonstrations, seminars, symposia, and inter and intradepartmental meetings. Through participation in symposia, CMEs, and journal clubs, they are exposed to contemporary developments. This will help them to focus on the aim, methods, remarks, conversations, and conclusions.
- They should gain clinical training by going through maximum clinical case discussions. Case discussions based on student-written patient records will assist students to hone their diagnostic and decision-making abilities.
- They should participate in presentations and discussions in a variety of ways. Using a problem-oriented approach will help students with decision-making.
- They should indulge in discussions with their senior postgraduate students before presenting in the symposium. The postgraduate students can prepare for a class-wide debate by participating in these discussions.
- Postgraduate students should indulge in bedside conversations during rounds and outpatient instruction which will help create an impact on patient management.
- Students should take interest in consultant’s case presentations which help in the solution of challenging issues and provide a forum for the debate of intriguing instances.
- The postgraduate students must take part in the training and instruction of interns and undergraduate students to brush up on their knowledge.
- They should attend monthly chat shows by eminent faculty, like the ones provided by the DigiNerve app.
- The student must take up rotations in the specialty clinics- Anterior segment and cataract, Glaucoma, Oculoplastics, Paediatric ophthalmology and strabismus, Retina and Uvea, Cornea, Contact lens and low vision, Neuro-ophthalmology, and Refractive Clinic.
- The postgraduate students should take the postings very seriously since they familiarize students with the typical ophthalmic issues. They must work freely and accept new and old cases, including refractions.
- The postgraduate student should make sure to keep an in-depth history and case record.
- MD students need to focus on basic sciences, biostatistics, research technique, teaching methodology, hospital waste management, health economics, medical ethics, and legal concerns connected to the practice of ophthalmology.
FAQs
Q1. What is the highest degree in ophthalmology?
Ans. Doctor of Medicine in Ophthalmology is the highest degree gained in the field of ophthalmology.Q2. What is the future of ophthalmology?
Ans. By 2025, there will be a need for about 22,000 ophthalmic surgeons, according to an estimate from the Health Resources and Services Administration in 2016. It also predicted that there will be more than 6,000 more doctors needed to meet the demand than there are currently available ophthalmologists.
Q3. What are the subspecialties in Ophthalmology?
Ans. Subspecialties in Ophthalmology include Glaucoma, Strabismus/pediatric ophthalmology, neuro-ophthalmology, anterior segment/cornea, retina/uveitis, oculoplastics/orbit, and ocular oncology.
COVID-19 has devastated families, institutions, and livelihoods while also scarring those at the front lines who witness it every single day. The strain put on our mental health during COVID-19 cannot be understated and the lockdown spent watching the news during such a time of extreme crisis has pressured our mental health further. It can be helpful to take moments out of your day to truly reflect on COVID-19’s impact on education and the mental health of students that might be fractured at the moment.
For those looking to pursue medicine, seeing crippling amounts of pressure being put on the healthcare system might be personally worrying. However, it is especially important to consider the mental health of students at such a critical juncture. To help take care of your mental health during covid-19, keep the following tips in mind to reduce stress.
- Free Headspace Subscription – Headspace is a US-based meditation app that announced a free subscription to all healthcare workers in India to tackle their mental health during COVID-19. Headspace has conducted numerous studies to reach the definitive conclusion that with just 30 days of guided meditation and practicing mindfulness, there has been a 30% stress reduction, greatly boosting mental health of students during COVID-19. If you are searching for a sense of peace in your days, consider signing up for Headspace.
- Take Care of Your Health – It can be difficult to separate your own life from those you care for but finding time to ensure that you are getting the exercise and nutrition you need is essential for myriad reasons. Firstly, an adequate diet that is supplemented with vitamins and nutritious food is essential to building up your immune system, an important factor when amid a pandemic. Secondly, as physical and mental health during covid-19 are interrelated, exercise regularly, try and sleep for full 8 hours, and eat healthy.
- Communicate Often – One of the best ways to destress and find a connection in an isolating time is to talk to other people. Be it friends, family, or a counselor, consider finding a connection and a way to unwind. Especially when considering COVID-19’s impact on the education and mental health of students during covid-19, these forms of socialization may provide a much-needed respite.
- Limit News – The endlessness of social media coupled with the stress of news can seriously harm the mental health of students during covid-19 and adults alike. While we all must remain alert about further developments in the pandemic, limit the amount of time that you ingest news.
If you find moments of solace through submerging yourself into challenging but rewarding tasks, perhaps signing up for an online course is a good way to spend your day. To get started, click here to view DigiNerve’s medical course options.
DigiNerve is an online medical education platform by Jaypee Brothers, and it is here to solve all the tutoring needs of medical undergraduate students, postgraduate students, and professionals. It aims to provide top-notch content to improve concept-building, acquire clinical skills, and crack exams by top-class faculty, accessible anytime, anywhere.
There are four categories of courses offered by DigiNerve: UnderGrad, PostGrad, Professional, and Exam Prep.
UnderGrad Category includes courses for 2nd, 3rd, and 4th year MBBS subjects:
- Microbiology for UnderGrads by Dr. Apurba S Sastry, Dr. Sandhya Bhat & Dr. Deepashree R
- Pathology for UnderGrads by Prof. Harsh Mohan, Prof. Ramadas Nayak & Dr. Debasis Gochhait
- Pharmacology for UnderGrads by Dr. Sandeep Kaushal & Dr. Nirmal George
- Forensic Medicine and Toxicology for UnderGrads by Dr. Gautam Biswas
- Ophthalmology for UnderGrads by Dr. Parul Ichhpujani & Dr. Talvir Sidhu
- Community Medicine for UnderGrads by Dr. Bratati Banerjee
- Pediatrics for UnderGrads by Dr. Santosh T Soans & Dr. Soundarya Mahalingam
- Orthopaedics for UnderGrads by Dr. Vivek Pandey
- Medicine for UnderGrads by Dr. Archith Boloor
- Surgery for UnderGrads by Dr. Sriram Bhat M
- OBGYN for UnderGrads by Dr. K Srinivas
Additionally, two combos are also available in the UnderGrads section,
- Basic Sciences Combo: This combo includes the second professional courses (Microbiology, Pathology, and Pharmacology) along with Clinics to provide them a clinical foundation in 2nd prof.
- Clinical Combo: This combo includes Medicine, Surgery, OBGYN, Orthopaedics, Ophthalmology, Community Medicine, Pediatrics and Forensic Medicine & Toxicology course.
PostGrad Category includes PG specialisation courses:
- OBGYN MD by Dr. Aswath Kumar
- Dermatology MD by Dr. Rashmi Sarkar & Dr. S. Sacchidanand
- Ophthalmology MD by Dr. N. Venkatesh Prajna
- Pediatrics MD by Prof. Piyush Gupta
- Medicine MD by Dr. Jyotirmoy Pal and Dr. Shashank R Joshi
- Surgery MS by Prof. (Dr.) Nilay Mandal
Professional Category includes the following courses:
- Ultrasound in OBGYN Made Easy by Dr. Sonal Panchal & Dr. Chaitanya Nagori
- Basics of Infertility & IUI Made Easy by Dr. Chaitanya Nagori & Dr. Sonal Panchal
- Ganga Videos on Spine Surgery by Prof. Rajasekaran Shanmuganathan, Dr. Ajoy Prasad Shetty & Dr. Rishi Mukesh Kanna
- Advance Course in Ultrasound and Infertility by Dr. Sonal Panchal and Dr. Chaitanya Nagori
- Critical Care Simplified by Dr. Yatin Mehta, Dr. Subhal Dixit, and Dr. Kapil G. Zirpe
- Organ Donation Simplified by Dr. Kapil G. Zirpe and Dr. Rahul Pandit
- Cosmetic Botulinum Toxin Simplified by Dr. Rasya Dixit, Dr. Urmila Nischal and Dr. K.C. Nischal
Exam Prep Category includes the following courses:
- Cracking MRCOG Part 1- Comprehensive Course by Dr. Richa Saxena
- Cracking MRCOG Part 1- Mock Exam by Dr. Richa Saxena
- Cracking MRCOG Part 2- Comprehensive Course by Dr. Richa Saxena
- Cracking MRCOG Part 2- Mock Exam by Dr. Richa Saxena
- Cracking MRCOG Part 3- Live OSCEs Engagement by Dr. Richa Saxena
- Cracking MRCOG Part 3- Non-Interactive OSCEs by Dr. Richa Saxena
- Cracking MRCP Part 1 by Dr. Gurpreet Singh Wander and Dr. Archith Boloor
Why Choose DigiNerve?
The course content offered by DigiNerve is not only as per the respective curriculums but is also brought to students easily and interactively. The courses include highly illustrative video lectures, competitive self-assessment questions, progress analysis, and specially curated notes while always focusing on concept-based learning. Here are a few other aspects of DigiNerve that set it as the best guide a student can have during their Top Doc journey:
- Esteemed Faculty: Each course on DigiNerve is curated and taught by Gold Standard Faculty in the respective field. For example, ‘Cracking MRCP Part-1’ is taught by the highly acclaimed Dr. Gurpreet Singh Wander and Dr. Archith Boloor, each of whom has published research papers and taught at renowned medical universities. Similarly, ‘Ultrasound in OBGYN Made Easy’ is structured and mentored by the distinguished faculty, Dr. Sonal Panchal and Dr. Chaitanya Nagori, who have years of expertise and have published successful books on gynecology. Also, UG courses such as Microbiology for UnderGrads is taught by the maestro himself, Dr. Apurba S Sastry along with Dr. Sandhya Bhat & Dr. Deepashree R, Pathology for UnderGrads by Prof. Harsh Mohan, Prof. Ramadas Nayak & Dr. Debasis Gochhait. These faculties already have an irreplaceable place on the shelves of every medical student. Thus, all students can be assured that no matter which course they choose, DigiNerve has got their back.
- Credible Content: Since all course content is structured by renowned faculty, all students get the latest medical breakthroughs, practically relevant material, clinical case demonstrations & discussions, and the benefit of over 50-year trusted medical legacy that Jaypee provides. All of this results in courses that have credible and valuable information to help students not only ace their medical and entrance exams but also develop their professional abilities as doctors.
- Easy to Use: DigiNerve is designed to be as student-friendly as possible. With an efficient and detailed website and a virtual classroom experience that is based on interactivity, all students can access courses and navigate with ease. Further, students can learn from their respective courses and content anytime and anywhere via the DigiNerve App. The app also has other great features, such as the Continue Journey Widget, Split View option to access the video lectures and notes simultaneously, Video Indexing, and ‘Ask a doubt’ feature.
- Specialization Courses: Apart from providing students with courses to help them crack competitive exams, DigiNerve also has specialized courses for doctors looking to hone in on a particular skill or for postgraduate students looking to enhance their practical knowledge. One such course is ‘Ultrasound in OBGYN Made Easy’. The course provides students with detailed knowledge of ultrasounds that is essential for gynecology and radiology practice. It also specifically teaches cutting-edge fetal medicine knowledge to help doctors reach a diagnosis.
- International Certification: On completion of the specialized courses offered in Infertility and IUI and Ultrasound in OBGYN, DigiNerve facilitates internationally recognized certificates for its students. Thus, boosting their CV, opening doors for higher pay and international practice in the respective specialization. For some courses like the USG course, students on completion receive a certificate from the prestigious Ian Donald Inter-University School.
DigiNerve is unparalleled in the quality of courses offered, the range of material taught, the Gold Standard faculty that structure and teach the courses, and the easily navigable interface. Thus, giving students helpful courses at a competitive price that provide them with conceptual clarity, allowing them to excel in their exams, and also offering practical guidance.